
Meniscus tears are very common. Each knee has two menisci which serve as cushions. They can tear due to degeneration, or they can tear due to trauma or a sports injury. The treatment of a meniscus tear will depend on the type of tear you have, whether or not you also have osteoarthritis and the nature of your complaints.
Many people do not understand why many meniscus tears do not require surgery. Having a firm understanding of what the meniscus does and why some tears do not require surgery should go a long way in assisting you in your surgical decision-making.
Meniscus tears are a very common source of pain in the knee. They are also commonly seen on MRIs obtained for other reasons – and are not necessarily the cause of your pain. Many people come in on a daily basis and ask if surgery for their meniscus tear is always necessary. In this post, we will explore
- what a meniscus is,
- what are meniscus tears,
- why meniscus tears are so common
Meniscus Tears
What is a meniscus? It is a cartilage disk that’s found in the knee.

There are actually two of them. We have one on the inner side of the knee which we call the medial meniscus and one on the outer side of the knee which we call the lateral meniscus. These two disks function as shock absorbers or cushions to minimize the stress on another type of cartilage that we have in the knee which we call the articular cartilage. The articular cartilage is the cartilage that actually coats the ends of the bones. If the two menisci are not present or they’re torn, then the articular cartilage sees an increase in stress and can trigger the onset of osteoarthritis. Meniscus tears are by no means the only cause of osteoarthritis. However, they certainly are a significant contributor.
Why do meniscus tears occur?
Now I see many patients every week who present with knee pain and many of them are suffering from meniscus tears. Why/How do we get meniscus tears? Why do these little meniscal disks tear so easily once we reach our fourth, fifth decades and beyond? Our meniscal tissue is non-regenerative. It’s similar to our brain or our heart tissues. If we have a heart attack or a stroke, we do not regenerate those areas of our heart or our brain. It simply scars in. Yet if we cut our skin, our skin heals. Our skin tissue is regenerative, same with some muscle and a lot of other tissues in our body.
The meniscus tissue in our knee has very few mechanisms for repairing itself. Therefore, every step that you’ve taken, every twist that you’ve done, every time you’ve knelt down or squatted down, you’ve put a force across that meniscus and eventually it wears out and the meniscus tears. (This is why most tears are referred to as being “degenerative”. A lot of times people will note that they simply knelt down to pick up something up and when they went to stand up they felt something rip inside their knee and noted the onset of pain.
Why does a meniscus tear hurt?
The typical patient with a meniscus tear doesn’t have much in the way of pain with walking straight ahead. Sometimes they do. It depends on the size of the tear but usually, they’ll tolerate walking in a single direction very well. Patients with meniscus tears will occasionally complain of pain going downstairs. They’ll have pain getting up from a seated position. They’ll have pain with turning, pivoting and twisting and some patients, if the meniscus tear is large will complain that the knee is buckling or giving way or feels unstable. Many of you will also find you need to sleep with a pillow between your legs at night.
A meniscus tear hurts because they sometimes irritate the lining of the knee joint called the synovium. Tears can also hurt if there is a loose piece which is getting caught in the joint.
Types of meniscus tears?
What are the different types of meniscal tears? The majority of tears are degenerative meniscal tears. When you look at the cartilage disc, the edges are simply frayed. The tissue has been destroyed from years and years of use. Nothing you did wrong. The tissue simply wore out. It’s like the front of a pair of blue jeans that you’ve worn for decades and the material just simply wore out.

Then there are those who have suffered more acute meniscus tears and these tears can have different shapes and different patterns. The shape and pattern will determine how symptomatic or how bothersome the meniscus tear will be. If a loose flap of tissue is created and that flap is moving around within the knee – that’s when you’re going to have given way and you’re going to have pain with many activities. You’re not going to tolerate flap tears well and those patients with flap tears (or unstable tears) will usually (not always) go on to require an arthroscopy or a scope to try to either repair or remove that torn piece.
We Treat Patients, NOT MRI findings…
Many patients with meniscus tear pain will improve within a few weeks of onset… in many cases, there is no need to rush into surgery.
- If your pain is starting to improve and
- if the pain does not interfere with your quality of life
- If compression sleeves work to control the pain
- If your range of motion is well maintained and
- You can participate in your normal daily activities —
Then why would one consider meniscus surgery a necessity? Not all “tears” require surgery. Again, we as physicians need to treat the patient, and not the disease.
Consider this article which demonstrated that a sham surgery (incisions made, but nothing done) was no better than treating a meniscus tear when the patient had a degenerative meniscus tear. There are also plenty of studies which show that a degenerative tear can be treated with physical therapy.
How are meniscus tears treated?
If you have knee pain, and you’re found to have a degenerative meniscus tear — I typically advise patients to simply just wait. A lot of times your symptoms will go away. If you sustain an injury and you have an unstable tear, a tear we call a horizontal cleavage tear, a radial tear or a flap tear — those are the tears tend to remain bothersome. If after four, five, six weeks, you still have the same degree of discomfort and quality of life issues, then you might be a good candidate for surgery, which we call an arthroscopy.
Physical therapy can help those of you whose knees feel unstable or weak, and it can help those of you with significant swelling to gain back your motion, stability and strength. Therapy can be beneficial before surgery (pre-habilitation), instead of surgery, or after surgery.
Many patients feel that a compression sleeve makes them feel better and improves their sense of stability – see some of our patients’ favorite knee compression sleeves here.
Do all meniscus tears require an arthroscopy?
What exactly is an arthroscopy?
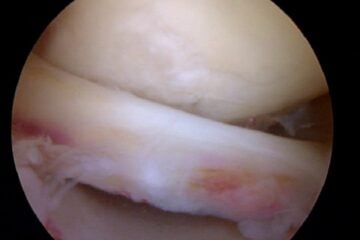
Basically, an arthroscopy involves bringing you into the operating room, inducing a light sleep, injecting local anesthesia and then placing a fiber-optic camera into your knee through a ¼ inch incision. We then inspect the entire joint, find the tear and determine if it will be removed or stitched back into place. Most procedures take 15-45 minutes and you are able to go home the same day. Whether or not you can return to sports soon will depend on which procedure you had — repair versus removal. More on the recovery from meniscus surgery here.
So if you have a meniscus tear, it’s not all doom and gloom. Many tears do not require meniscus surgery. Some of them do. Some meniscus tears are repairable. Sometimes the torn portion of the meniscus is simply removed.
We try to repair – or suture- meniscus tears whenever possible — but only certain tears are in fact repairable. One caveat: If you have a meniscal tear and you’re experiencing instability or giving way, be very careful with your activities. You don’t want to find yourself on the stairway carrying a load of objects and your knee gives way. If you have instability symptoms, make sure that you have a hand available to hold onto something at all times while you are in your recuperative phase or awaiting surgery or simply waiting to see if the symptoms are going to recover on their own.
Hope you enjoyed this post. For more information there is a more in depth section on meniscus tears here.
And by no means is meniscus surgery or emergency surgery. Take your time, rest and consider a second opinion.
After your meniscus surgery, what should you expect as your recovery from an arthroscopy for a meniscus tear?
Due to the overwhelming popularity of this post, I want to make sure that the many and varied needs that each of you have is met during your visit here. With that in mind, you may benefit in reviewing these related posts on this site:












Dear Dr. Luks,
I am a 29 yrs old male, fit and have been playing soccer for many years.
I injured my right right knee after playing soccer recently, it was painful and swollen initially. It has been 10 days now since the injury and it is still swollen – though less swollen that before – and the pain has reduced, though I cannot squat my right leg fully, and pain will be stronger if I am to move my leg in certain ways – including sudden movements. I had an MRI scan which showed the following:
“Within the medial compartnment there is a large horizontal tear of the body and posterior horn of the medial meniscus extending to the inferior articular surface. The Chondral surfaces are preserved with no focal defects. The medial collateral ligament is intact. Mild bone oedema is present in the medial tibial plateau.
Within the lateral compartment the lateral meniscus is intact. The Chondral surfaces are intact with no defects. The posterlotaral corner structures are unremarkable.
Within the patellofe,oral compartment the chondral surfaces are preserved with no focal defects. The quadriceps and patellar tendons are intact.
The anterior and posterior cruciate ligaments are intact. A large join effusion is present. There are no intra articular loose bodies. There is no Baker’s cyst.”
I am scheduled to see the specialist – orthopedic surgeon – soon, but it seems I would need a surgery (orthoscopy) done… Do you think this is the case with certainty, based on the MRI findings?
Many thanks for the assistance and the response in advance.
Kind Regards
It’s possible Anas… but keep in mind. Many of us might repair a tear like that at your age. It might be hard to find someone to repair it as opposed to removing the torn piece. Do your research and seek a few opinions if necessary.
Hey,
I am a 24 year old male who is extremely fit. I have been playing soccer since I was 6 years old pretty much. I just wanted an opinion on my MRI report before I discuss this issue further with all the medical professionals. I have been working as a car detailer for the last 2-3 years pretty much full time and over these last few years I have had 2 injuries to my knee when I was off season from soccer where the inside of my right knee would hurt a lot from all the twisting I did on my knee getting in and out of cars over 200 times a day (it would only put me out of soccer and work for a week). Anyways towards the problem, 2 weeks ago I slipped over while playing indoor soccer and I heard a few pops in my knee. It swelled up over the next few hours and for about a week I struggled to get out of my bed with pain and swelling and limited movement of my knee. Its 2 weeks later now and my swelling has significantly improved and I am able to move my knee around a lot more without the pain.
I just picked my MRI report and this is what it said,
patella and supra-patellar recess
the articular cartilage appears within normal limits for the patients age. there is a moderate knee joint effusion. there is a small amount of fluid in the deep infrapatellar bursa
anterior cruciate ligament
there is increased signal intensity and irregular contour of the anterior cruciate ligament indicative of strain injury
Posterior cruciate ligament
there is normal signal intensity and contour of the posterior cruciate ligament
medial meniscus
there is evidence of increased horizontal signal extending to the inferior articular meniscal surface in the posterior horn and a vertical component in the anterior horn extending to the articular surfaces, involving the annular fibres
lateral meniscus
there is no evidence of increased signal extending to the articular meniscal surfaces indicative of a meniscal tear
medial collateral ligament
there is increased signal intensity adjacent to the medial collateral ligament in keeping with a grade 1 strain injury
lateral collateral ligament
there is normal signal intensity and contour of the lateral collateral ligament
medial compartment and lateral compartment
the articular cartilage appears within normal limits for the patients age
femur and lower leg bones
there is a focally increased T2W signal intensity of the bone marrow of medial femoral condyle and medial tibial plateau indicating bone oedema secondary to a medial compression injury
Comment:
there are features of a complex medial meniscal tear as described
And on a seperate X-ray they found that my hoffa’s fat pads had some soft tissue swelling.
Do you think surgery will be necessary?
HI Antoni..Hard to say if surgery is the answer. Last thing you want to do is loose part of your meniscus at your age. Many doctors recommend physical therapy, etc for a short while before determining if surgery is necessary. In addition, keep in mind that many surgeons, myself included might be able to repair (sew back together) horizontal tears as opposed to trying to remove the torn portion. Try to find a surgeon who is willing to give it a go if it is possible. The decision to repair vs remove is actually made during surgery .. but many products, like the Centrix repair device have made it easier to repair certain tears. Good Luck
Howard Luks
Dear Dr. Luks,
last August I injured my right knee when playing football. On 30th August, 2013 I had a surgery – ACL reconstruction and repairs on both menisci. There were two tears in each meniscus. After the surgery I was on crutches for 30 days with no weight bearing on the “repaired” leg. Since than I have been doing rehab and working out for muscle strength. Gradually I started running and got to running 4 km without any pain in the knee :)
I also started doing some plyometric exercises – like box jumps with both legs. At 8,5 months after surgery I decided to start one leg jumps. One they I did 3 sets of 10 reps jumps with each leg. Right after that I ran another 4 km. I was feeling well at the end of the work out – no pain at all.
However, on the next day my knee felt stiff and flexing was more difficult than before, although I was able to flex both legs almost equally. It’s been almost two weeks, I have been resting, the knee is not stiff any more and flexing is fine, however, sometimes I feel slight pain when walking. I am worried that I did something to the repaired menisci with these one leg jumps… :( Is this possible or its just that this exercise introduced a completely new type of stress to the knee (after almost 9 months) and the muscles around the knee need some time to recover and get used to it?
Next week I will see my orthopedist to discuss this issue with him, but I have been really down and worried that I have injured myself again. I would really appreciated Your opinion.
Thank You in advance!
Kind regards,
Mladen
It’s not unusual for a reconstructed knee to respond to a new activity like this. Hopefully your exam shows that all is well.
Good Luck
Howard Luks