
Millions of people suffer from degenerative joint disease (DJD), or osteoarthritis(OA) of the knee. Degenerative joint disease of the knee is the cause of significant pain and disability. Many people do not clearly understand what degenerative joint disease is. Perhaps your doctor said, “It’s just degenerative changes”. That’s all well and good, but your knee hurts, and you do not know what your next steps are. Many questions need to be addressed.
- What is Degenerative joint disease?
- How do I treat it?
- Why does it hurt so much? Should I continue to exercise (see video below)?
- Will exercise make my degenerative joint worse (see video below)?
- Are there non-surgical alternatives to treat knee DJD?
- Do I need surgery for my knee arthritis?
Let’s start first with the causes of degenerative joint disease and then proceed with the commonly accepted, reasonable treatment alternatives available for joint pain sufferers. Any decision you make should be based on your quality of life … and not your X-ray or MRI findings. We treat patients… not MRI or X-ray findings!
What is degenerative joint disease?
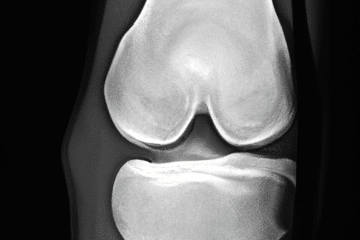
Degenerative joint disease, also known as osteoarthritis is due to the loss of cartilage within your joints. The articular cartilage is the cushioning that is on the ends of our bones. When we finish growing, that cartilage is fairly thick, it is firm and rubbery … and smoother than glass. For many reasons, we start to lose the cartilage, or we may suffer an injury which will cause us to lose our cartilage.
The causes of degenerative joint disease are numerous, some of the more common causes are:
- genetics — do you have a family member with arthritis?
- trauma — injuries can start a degenerative cascade to occur.
- nutritional — some think that vitamin D deficiency can cause arthritis
- mal-alignment — Are you bowlegged or knock-kneed?
- meniscus tears: loss of meniscus function (as a shock absorber) can lead to arthritis
Why does degenerative joint disease hurt?
If you lose enough cartilage or cushioning on the ends of your bones, then the bone underneath the cartilage will experience more stress. A degenerative joint disease is, by definition, a loss of cartilage. Our cartilage can wear thin over time, even without any specific injury to a joint. The most common causes of arthritis include genetics …. do your parents have it? Knee joint arthritis can also be caused by previous injuries, previous surgery, meniscus tears, ACL tears, and other more rare diseases.
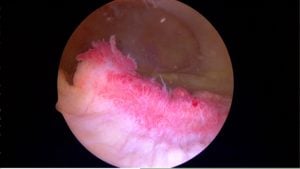
The pain due to DJD is caused by inflammation, or “synovitis.” Therefore, managing the pain of osteoarthritis is all about managing the inflammation or “synovitis”.
The synovium is the tissue which lines the entire inside of our joint. Usually, the synovium is thin and produces just enough fluid to allow our joints to move without pain or friction. In patients with degenerative joint disease or osteoarthritis, the synovium can become inflamed. That inflammation itself is the cause of significant pain. If the synovium is inflamed it may manufacture more fluid than normal and that’s why many of you have a warm, swollen knee — or as you may refer to as “water on the knee”. The most common cause of knee swelling is osteoarthritis. The latest non-surgical procedure available arthritis pain sufferers is a selective arterial embolization. It works by decreasing the inflammation within the knee by minimizing the blood supply to the synovium. The early results have been very promising. If interested read our post on arterial embolization for knee arthritis.
If your bones are not protected by cartilage they may experience more stress. That stress can lead to stress reactions or stress fractures which can cause severe pain. If you have had an MRI and they mention bone marrow edema — that means fluid or inflammation in the bone itself. Bone marrow edema is a common source of pain. If your X-rays do not show bone on bone arthritis, but you have bone marrow edema, then a procedure called a subchondroplasty might ease your pain significantly.
Can I exercise if I have osteoarthritis?
The video below shows the other list of treatments our patients utilize to treat their knee pain.
Degenerative joint disease treatments
Treatments and recommendations vary depending on how severe your pain is, your age, your activity level, and any other medical problems you may have.
Note: Any medication or supplements mentioned should be reviewed with your primary care doctor before starting them since they can interact with other medicines or they may not be indicated because of an underlying medical problem you have.
- Lifestyle changes: Many people will experience relief from simply slowing down. Shorter walks, shorter runs, switching to a bicycle or swimming for exercise etc. Keep track of your activity. Try to increase your walking and aerobic capacity. Consider a Fitbit to monitor your activity. These trackers are great for helping you stay on course. Research has shown that exercise, specifically light weights or resistive training can minimize the pain of osteoarthritis or degenerative joint disease.
- Weight loss: I know, I know… BUT … for every one pound you lose, you will take 4-7 pounds of force off your knee!! Therefore even a relatively small weight reduction will result in significant pain relief. I have had many people cancel their knee replacement surgery after they lost 20-30 pounds.
- Braces or sleeves: Compression sleeves can provide meaningful relief of pain for many. We believe that compression sleeves improve knee pain because of a biofeedback mechanism. When you purchase one, if it is tight enough to stay on, it is tight enough… do not get a sleeve that is too tight. In this post I review the compression sleeves I see most commonly in the office.
Supplements and Vitamins
*Note: Many now believe that supplements have little role in managing knee pain. Despite that, the most popular supplements our patients are taking include:
- Vitamin D: Get tested. Know your level.
- Curcumin: Curcumin has many anti-inflammatory properties.
- Fish Oils: Fish oils contain chemicals which act in a similar way that aspirin or other NSAIDs do. Check with your doctor first since in can interact with other medications. Here is a rather scientific, but complete description of the benefits and side effects of fish oils and why they might work.
- glucosamine/chondroitin sulfate: Chondroitin Sulfate is the most commonly taken supplement. Some recent research shows that it may work to limit pain… but it will NOT regrow cartilage. A recent roundtable discussion among Orthopedic Surgeons show that they would take it too.
- Tart cherry juice There are many patients I have seen who enjoy the benefits of tart cherry juice.
Selective Arterial Embolization
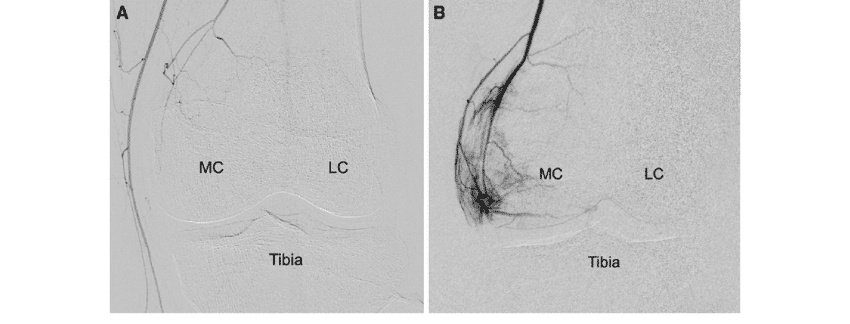
The pain of arthritis is often due to inflammation of the lining of the knee joint. That inflammation is often due to the fact that your body grew too many new tiny blood vessels to nourish the synovium around the swollen and arthritic areas of your knee. Recent research shows that selectively eliminating those extra blood vessels can lead to nearly complete relief of the pain from arthritis for 6 years or more.
- Injections: Nobody likes to receive an injection… and yes, they hurt — but they might give you significant relief. The options available to us include:
- Cortisone or steroids. These potent anti-inflammatories once injected will usually result in significant pain relief which can last for a few months. You must check with your physician first about potential interactions with other medications. If you are a diabetic, cortisone injections WILL make your blood glucose rise!
- Hyaluronic Acid : Examples include Synvisc, Orthovisc, Hyalgan, etc… Many people refer to these as gel injections. Some people mistakenly believe they are cartilage injections. They are not. Hyaluronic acid injections might improve your pain for upwards of 4-8 months. They are effective for most people… but not everyone.
- Platelet Rich Plasma or PRP: PRP is prepared by collecting a sample of your blood, placing that sample into a centrifuge and then taking off a certain layer and injecting it into your knee. Recent scientific literature shows that it may work to limit your pain significantly . PRP, or platelet-rich plasma injections, involve the injection of your own concentrated platelets, protein-releasing bodies, and other healing growth factors that can aid the body in resolving certain inflammatory conditions and can heal worn out tissues. It is an office based procedure where a small amount of blood is collected from you — the sample is prepared in a special apparatus placed into a centrifuge and then injected back into the site to be treated. In prior years PRP was investigated for the treatment of tendon-related disorders such as tennis elbow. PRP has received a lot more attention recently as an alternative to minimize or alleviate the pain associated with arthritis of the knee. In a recent study published in the The American Journal of Sports Medicine it was shown that PRP or Platelet Rich Plasma was effective for alleviating or improving the pain from arthritis of the knee. Further studies have shown that PRP injections may slow the progression of your osteoarthritis.
- Exercise: Resistance exercise and Minimal impact exercises such as rowing, swimming, and walking help alleviate the pain of arthritis and improve the strength of your legs… and your heart will be happier too. The research is also very clear in this area. Exercise will not make your arthritis worse. Perhaps exercising too much might cause more pain, but that does not mean that you are causing arthritis to become more severe. The research has also shown that people who remain active, and actively exercise are able to delay surgery for their degenerative knee pain for many years.
- Physical therapy: Either physical therapy, a pool program, or a gentle land-based exercise program can improve your pain and delay the need for more aggressive treatments. For those of you who are looking to start an exercise program than starting with a trained professional such as a physical therapist is a great place to start. Again, physical therapy is not going to cure your arthritis or degenerative joint disease, but for most of you it will improve your pain and thus improve your quality of life.
- Surgery:
- Arthroscopy: Tread lightly when someone recommends an arthroscopy or “scope” to “clean out” an arthritic joint. The results are usually poor, and the research is fairly clear that arthroscopy has a very limited role in the management of degenerative joint disease… at best. Most insurers and Medicare will not cover the surgery if the primary diagnosis is osteoarthritis.
- High Tibial Osteotomy: This is a procedure offered to young patients with arthritis limited to one side of the knee joint. It involves cutting the tibia and changing the alignment of the leg to take the pressure off the side of the knee that is arthritic. Visit this page for more information about a high tibial osteotomy.
- Knee replacement: Knee replacement is, unfortunately, the only definitive procedure we have to “treat” degenerative joint disease which has not responded to other treatments. Here is an interesting video to see. It is a video from a patient, where they offer their perspective on a knee replacement procedure. If the pain and disability is significantly interfering with your quality of life then a knee replacement might be a good option for you. Knee replacements can be partial, or “total”. A knee replacement is a big procedure, and you are a key member of the team. You need to be physically and emotionally prepared for your knee replacement, ready to assume the risks of surgery and be ready to work hard in rehabilitating your new knee. You need to find a surgeon who does a reasonable volume of joint replacement and doesn’t dabble in joint replacement surgery … volume matters and diminishes the risks of complications in knee and hip replacements. The NY Times published an opinion piece on the issue of the treatment of osteoarthritis and knee replacements that you may wish to review.











hi im a 40 year old woman with this condition but my counsultant wont do anything all i was told was to lose some weight and some physio …. ive been suffering for over 6 years now i tried to lose weight but my chrons disease is making me put on weight is there anything i could try to ease the pain and stop the locking and cracking .
Did you try the physio? Perhaps a compression sleeve? Chondroitin Sulfate? You may even want to try the HA injections too. I can not make any formal recommendations without see you in the office first.
Good Luck
I am a 52 year old man who has had 2 scopes done on my right knee when I was in my 20’s. I have been having increased pain over the past few years. I had a cortisone shot that did more harm that good. I recently had an MRI and here are a portion of the results:
FINDINGS: “Moderate degeneration with chondrocalcinosis medial meniscus. Mild fibrillation fraying noted of the free edge. Chondrocalcinosis also noted of the lateral meniscus. There is studding of low signal intense calcium deposit within the cartilage of the lateral knee compartment. Articulating cartilage caliber of the lateral and medial knee compartments otherwise intact. Mild chronic sprain and thickening superior tibial collateral ligament. Similar-appearing low signal intense calcium studding noted of the medial patellar facet articulating cartilage. Mild marginal osteophytes patellofemoral joint. Minimal lateral patellar subluxation and tilting noted.”
I exercise 3 to 4 times a week and have lost over 40 pounds in the past 2 years. Labs show normal levels in all categories.
General Thoughts? I hope I won’t need a new knee, but if it gets rid of the pain, I may consider it.
CPPD can cause pain, especially if arthritis is present too. Not sure what your question was.
I had surgery to repair a torn SCI and complete meniscus tear about six years ago. I’m overweight and have recently started to increase my activity level. I’m finding that I have significant discomfort after exercising and pain in the front inside of my knee when I bend at the waist. Does this sound like o set o f arthritis?
It is possible… it is also possible that your thigh / and hip muscles are weak.