
Degenerative meniscus tears are very common. Many adults over 55 have one and will not know it. Surgery for degenerative meniscus tears is rarely necessary. Most research shows that people do just as well with physical therapy. This post will carry two messages, both equally important. First, surgery is rarely necessary for degenerative meniscus tears. Perhaps even more important is that once your knee feels better, and it may take several months, you should try to return to your normal activities.
Think about this second statement for a moment. If you had an episode of knee pain, and you had an MRI which revealed a degenerative tear; even though you now feel better you may not return to being active because you are afraid of harming your knee. Arthritis and other conditions worsen, even if you are at bed rest. Meniscus degeneration and tearing are no different. It is more of a biological issue than a mechanical issue. Meaning that you cannot stop the process, so you might as well remain active.
Why would you want to slow down your activities which are decreasing your risk of diabetes, obesity, dementia, hypertension, heart disease, and stroke? Rest comes with a heavy burden with respect to your overall health.
Recent research about degenerative meniscus tears and surgery:
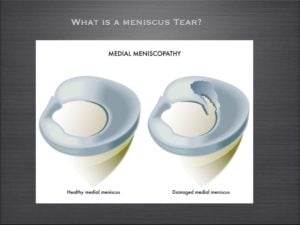
The meniscus is a cushion inside your knee. It aids in the stability of the knee and minimizing the stress across the knee, thus minimizing the risk of developing osteoarthritis.
Meniscus tears are incredibly common. Although meniscus tears occur in all age groups, they are most common in adults over 55. There are many different types of meniscus tears. By far the most common tear is a degenerative tear of the posterior horn of the medial meniscus.
An article published in the New England Journal of Medicine out of Finland studied patients with degenerative meniscus tears. They studied whether the results of an arthroscopy (surgery) was better than a sham surgery (where the patient is brought to the operating room and thinks they had the surgery).
As published in the NY Times, The authors found …
A popular surgical procedure (arthroscopy) worked no better than fake operations in helping people with one type of common knee problem (degenerative meniscus tear), suggesting that thousands of people may be undergoing unnecessary surgery.
The Wall Street Journal posted a similar article, and led off by saying…
A fake surgical procedure is just as good as real surgery at reducing pain and other symptoms in some patients suffering from torn knee cartilage
These findings are not new, but in this environment perhaps they will shine a light on the over-treatment of degenerative meniscus tears. In 2007 a study showed that the results from an arthroscopy for a degenerative meniscus tear were not superior to a supervised exercise program.
What is a degenerative meniscus tear?
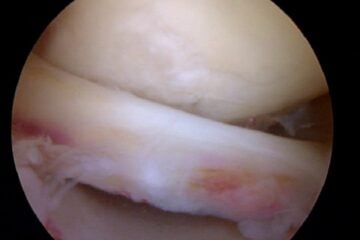
Degenerative tears occur because as we age, or because of our genetics — our tissues simply wear out over time. A degenerative tear is frayed, worn out tissue that looks like the worn out area on the front of your blue jeans. It has very little character, and the tissue is thin, soft, flexible, and looks worn out when we view it at the time of surgery. Most of these changes we see in the meniscus we consider to be “age-appropriate.” We accept thinning hair, the need for glasses, slower running times, and so on… but none of us expect that our internal structures are showing signs of aging too.
For many many years, I have spoken to people about the fact that many meniscus tears, especially degenerative meniscus tears do not often require surgery.
Do I Need Surgery For a Degenerative Meniscus Tear?
Many patients are under the assumption that because something is torn, therefore it must be fixed. That is not the case for many issues in Orthopedic Surgery. This paper on the non-surgical management of degenerative meniscus tears versus surgical management is yet another in a series of papers that supports the non-surgical management of degenerative meniscus tears, especially in the setting of osteoarthritis. Despite how severe your pain is at the onset of your symptoms, typically within a few weeks, your knee feels much better if managed by physical therapy, ice, heat, and anti-inflammatory medication (if you tolerate it).
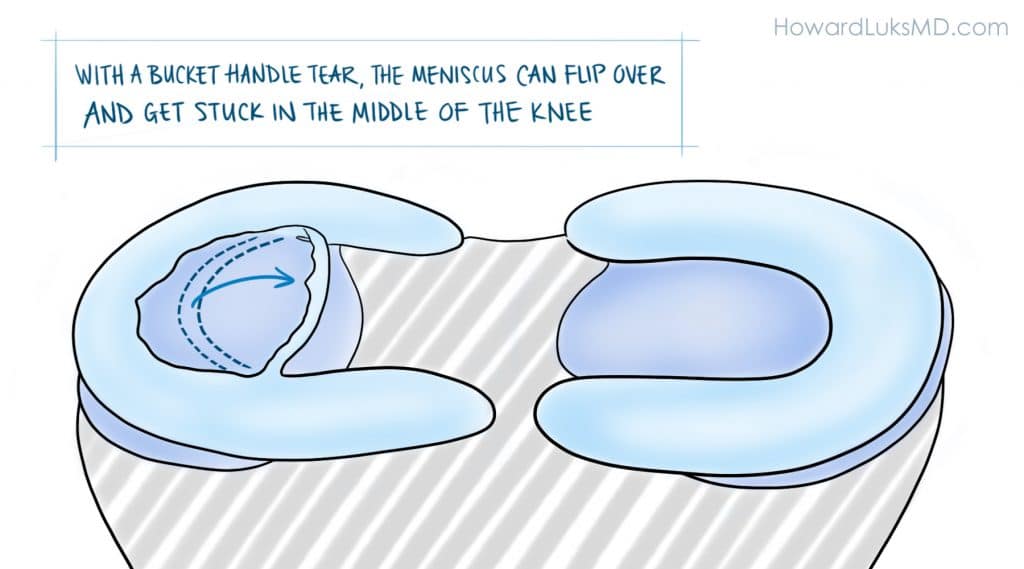
It must be pointed out. The authors of the paper studied degenerative meniscus tears. They did not study the more unusual “radial”, “flap”, or “bucket-handle” tears that can occur in the meniscus. These other tears can be far more “unstable” and produce mechanical symptoms such as instability, buckling, and giving way. In those instances, a meniscal repair, or removal of the torn flap will more than likely be necessary.
This was an important article about the management of this type of meniscus tear, but more studies are necessary. The take-home message is simply that all meniscus tears do not need surgery. Degenerative meniscus tears are usually managed well without surgery.
Have realistic goals about your recovery.
Very few of your orthopedic issues will resolve in less than 3 months. Many of you were told that if your pain persists for 4-6 weeks you should consider surgery. I would suggest that you wait longer than that. With 25 years of treating people under my belt, I can tell you that the majority of people were glad that they waited longer before moving forward with surgery. Surgery might actually bring you closer to a knee replacement. Surgery for degenerative tears will not decrease your chances of developing osteoarthritis. If you do choose to proceed with surgery for a degenerative meniscus tear it should be because:
- your pain persists after a lengthy period of non-surgical management,
- it was a quality of life decision…
- and your surgeon told you that you have little or no arthritis in your knee.
When your visit with your doctor be sure to ask what type of tear you have. If you possess a degenerative tear, without any of the “mechanical” symptoms we mentioned — you should pursue non-surgical treatment at first— and a few months later I think you’ll find that you’re glad that you did.












I am a 53 year old male. I have been exercising regularly for the past 15 years hoping this would help me not to follow the same destiny than my mother who had severe osteoarthritis at a much younger age. A few weeks ago I started to have a significant pain in my right knee. Besides a regular regime of daily soft exercise, I used to run 10 Km every Saturday. I thought that limiting it to a once-per-week frequency would help me keep my joints healthy while enjoying all the joy of jogging a relatively long distance.
But after I developed the pain, I went to see my doctor and he ordered an MRI. In the MRI they saw a horizontal grade 2 tear in the medial meniscus with still a normal thickness in the cartilage.
My doctor told me to wait and see doing a little bit of swimming and taking NSAIDs.
I would like to ask you how can I interpret the finding in the MRI in layman terms. I mean, does a horizontal tear is a worse case than a radial or a complex tear? What does grade 2 implies?
Thank you for posting your comments and the video. They are of great help.
Victor Joubert
A grade II signal is not a tear … it is within the inside of the meniscus, typically due to degeneration or a tear that might be just starting. Many horizontal tears and radial tears are repairable … wouldn’t worry much now…. sometimes these grade II signals stay like this for years. Good Luck
Hi again Dr Luks,
I wrote a comment earlier, mid October, about my knee. I had a MRI again which stated no change and no meniscal damage, but was still having symptoms. I then had a MR-arthrogram which revealed a incomplete meniscal capsular separation of the superior portion of the medial meniscus posterior horn. I suspect I originally tore it 3 years ago, but the pain resolved and I was able to return to sports in 2 months. 2.5 months ago, I felt a small tear while running and suspect that’s when I reinjured it. I am unsure if I retore a previously healed meniscus or if simply tore more of the original tear that never healed. Either way, I still have pain at night, with walking…pretty much all the time I feel either throbbing, stabbing, tightness or achy ness. Guess those are bad symptoms because there is blood flow to the area. I believe the tear is surgically repairable, but my concerns are this: it has been such an old tear ( though with a more acute episode with likely larger tear now) and I am unsure it would scar down. 2nd, while placing sutures in for the repair, one would have to make an incision and could this possibly result in a new tear? I have had one dr ( not a surgeon, but is a sports med ortho dr) say wait it out as it is unlikely it will heal and another tear could occur from surgery. While I have had another ( surgeon), say to repair. Last year I also had a different ortho surgeon say he wouldn’t operate on me, but at the time we didn’t know I had a meniscal capsular separation injury. What do you think is the best route for maintaining longevity of my meniscus. I really appreciate the help! I am so confused what to do:/
Meant to say blood flow aren’t bad symptoms:) also, I am 30 years old….so I know I’m starting to not heal as good as younger individuals!
One more thing! Besides pain with valgus positions and tibial ER in a more extended position, I have pain with Sagittal movements. I am unable to perform hamstring stretches or hamstring strengthening as I get medial joint line pain. Also, if I try to run ( complete straight line on level ground), I have pain sharp pain if I heel strike but sometimes no pain if I run more forefoot or up uphill on a incline. Would these symptoms correlate with a meniscal capsular injury? Thank you for your insight!
Last thing:) re-reading my reports it states MRI from 2014 had about a 10mm tear, MRI 11/2015 said no tear, MRA 11/2015 said about 15 mm tear. Don’t know if comparing MRI to MRA can truly show the change in tear. Btw, I absolutely agree with you how physical examination can be more accurate than imaging!