
Degenerative meniscus tears are very common. Many adults over 55 have one and will not know it. Surgery for degenerative meniscus tears is rarely necessary. Most research shows that people do just as well with physical therapy. This post will carry two messages, both equally important. First, surgery is rarely necessary for degenerative meniscus tears. Perhaps even more important is that once your knee feels better, and it may take several months, you should try to return to your normal activities.
Think about this second statement for a moment. If you had an episode of knee pain, and you had an MRI which revealed a degenerative tear; even though you now feel better you may not return to being active because you are afraid of harming your knee. Arthritis and other conditions worsen, even if you are at bed rest. Meniscus degeneration and tearing are no different. It is more of a biological issue than a mechanical issue. Meaning that you cannot stop the process, so you might as well remain active.
Why would you want to slow down your activities which are decreasing your risk of diabetes, obesity, dementia, hypertension, heart disease, and stroke? Rest comes with a heavy burden with respect to your overall health.
Recent research about degenerative meniscus tears and surgery:
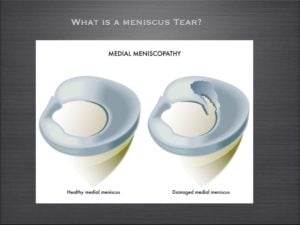
The meniscus is a cushion inside your knee. It aids in the stability of the knee and minimizing the stress across the knee, thus minimizing the risk of developing osteoarthritis.
Meniscus tears are incredibly common. Although meniscus tears occur in all age groups, they are most common in adults over 55. There are many different types of meniscus tears. By far the most common tear is a degenerative tear of the posterior horn of the medial meniscus.
An article published in the New England Journal of Medicine out of Finland studied patients with degenerative meniscus tears. They studied whether the results of an arthroscopy (surgery) was better than a sham surgery (where the patient is brought to the operating room and thinks they had the surgery).
As published in the NY Times, The authors found …
A popular surgical procedure (arthroscopy) worked no better than fake operations in helping people with one type of common knee problem (degenerative meniscus tear), suggesting that thousands of people may be undergoing unnecessary surgery.
The Wall Street Journal posted a similar article, and led off by saying…
A fake surgical procedure is just as good as real surgery at reducing pain and other symptoms in some patients suffering from torn knee cartilage
These findings are not new, but in this environment perhaps they will shine a light on the over-treatment of degenerative meniscus tears. In 2007 a study showed that the results from an arthroscopy for a degenerative meniscus tear were not superior to a supervised exercise program.
What is a degenerative meniscus tear?
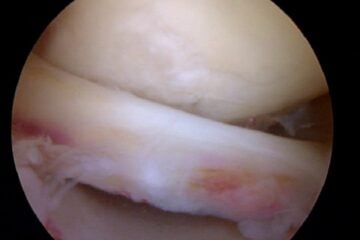
Degenerative tears occur because as we age, or because of our genetics — our tissues simply wear out over time. A degenerative tear is frayed, worn out tissue that looks like the worn out area on the front of your blue jeans. It has very little character, and the tissue is thin, soft, flexible, and looks worn out when we view it at the time of surgery. Most of these changes we see in the meniscus we consider to be “age-appropriate.” We accept thinning hair, the need for glasses, slower running times, and so on… but none of us expect that our internal structures are showing signs of aging too.
For many many years, I have spoken to people about the fact that many meniscus tears, especially degenerative meniscus tears do not often require surgery.
Do I Need Surgery For a Degenerative Meniscus Tear?
Many patients are under the assumption that because something is torn, therefore it must be fixed. That is not the case for many issues in Orthopedic Surgery. This paper on the non-surgical management of degenerative meniscus tears versus surgical management is yet another in a series of papers that supports the non-surgical management of degenerative meniscus tears, especially in the setting of osteoarthritis. Despite how severe your pain is at the onset of your symptoms, typically within a few weeks, your knee feels much better if managed by physical therapy, ice, heat, and anti-inflammatory medication (if you tolerate it).
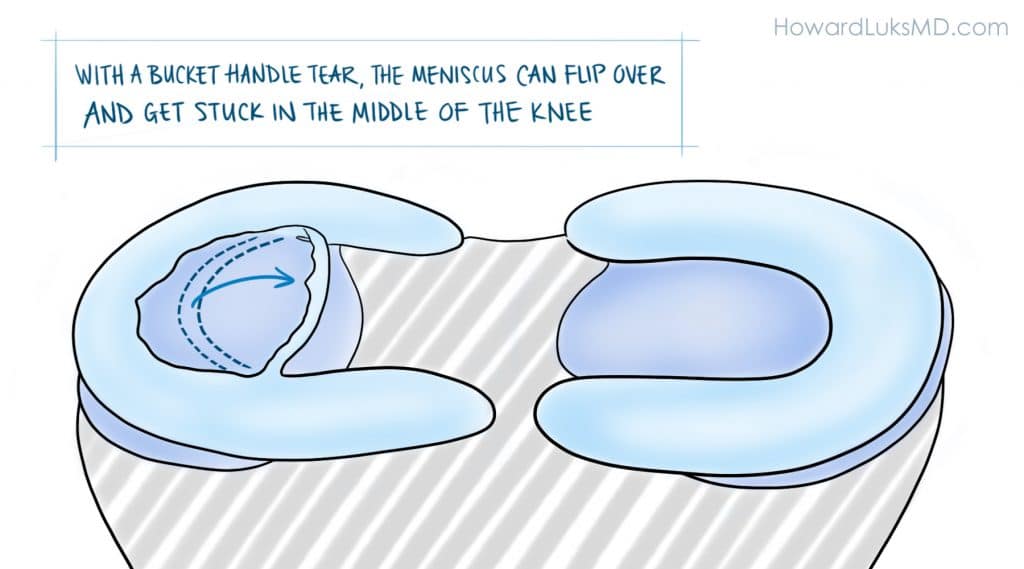
It must be pointed out. The authors of the paper studied degenerative meniscus tears. They did not study the more unusual “radial”, “flap”, or “bucket-handle” tears that can occur in the meniscus. These other tears can be far more “unstable” and produce mechanical symptoms such as instability, buckling, and giving way. In those instances, a meniscal repair, or removal of the torn flap will more than likely be necessary.
This was an important article about the management of this type of meniscus tear, but more studies are necessary. The take-home message is simply that all meniscus tears do not need surgery. Degenerative meniscus tears are usually managed well without surgery.
Have realistic goals about your recovery.
Very few of your orthopedic issues will resolve in less than 3 months. Many of you were told that if your pain persists for 4-6 weeks you should consider surgery. I would suggest that you wait longer than that. With 25 years of treating people under my belt, I can tell you that the majority of people were glad that they waited longer before moving forward with surgery. Surgery might actually bring you closer to a knee replacement. Surgery for degenerative tears will not decrease your chances of developing osteoarthritis. If you do choose to proceed with surgery for a degenerative meniscus tear it should be because:
- your pain persists after a lengthy period of non-surgical management,
- it was a quality of life decision…
- and your surgeon told you that you have little or no arthritis in your knee.
When your visit with your doctor be sure to ask what type of tear you have. If you possess a degenerative tear, without any of the “mechanical” symptoms we mentioned — you should pursue non-surgical treatment at first— and a few months later I think you’ll find that you’re glad that you did.












Thank you Dr. Luks for the most informative site I think I have ever visited! Saw my orthopedist today, and while I am unable to provide the extensive details of some of the other sufferers, I can say he told me I have a compound tear in my medial meniscus and suggests surgery to remove the flap. I had a previous tear in the other knee and had Synvisc treatment that was miraculous! I mentioned this and he agreed we would try this action first. What is your feeling? BTW,I am 57 years old. Very active. I just got back from running 5 miles at the gym , which I do about 4-5 times a week in addition to some weight lifting.
Thank you for the kind comments. If you are running and active, then you have many non-surgical choices before you. Surgery should be your last choice… it comes down to a quality of life decision.
Good Luck !
Hi Doctor Luks,
I have found your website perhaps the best on the web for understanding options on meniscus tears. Thank you. It seems a tear can be a life changing injury, but there are a lot of unknowns about this injury.
Unlike some, I have really tried to look after my knees (giving up soccer years ago and not ever running more than 10 miles and that cross country). But still at 46 I started to get real pain (Synovitis) in both knees then after a 3 mile run big swelling that was diagnosed in 2013 as;
a medial inner third vertical tearing damage.
After a bit of physio I was offered an operation but declined. The knee never felt right (didn’t feel up to running or jumping) and sometimes twisting on would lead to sharp pain and collapse but only once or twice. Did my best to look after it (even more bone broth!), stopped doing multi-day mountain walks and running. At this point I could fully squat, climb stairs not problem. A second MRI found in April 2015:
Medial Meniscus: oblique tear of the posterior portion with a separated and unstable fragment.
Now, 49 I have had intense pain 2 days after a 3 hour steep mountain walk- the first in 6 months. I could not really walk on it. The joint is fairly flexible only the last 10-15 degrees is painful, but the pain on walking constant and vulnerable to any twist (particularly at night – when it wakes me up) and the pain at that point is extreme. It has got better over 4 days, but I still walk with a feint limp. The consultant said it looks like I am getting closer to an operation and pain will be a recurring thing and I can swap pain now for arthritis later.
Questions: With an operation (say 10% removal) really end up in arthritis despite giving up all the stressful activities and just sticking to walking, cycling and swimming. I do want to walk in wild mountainous places though.
Is there any point in delaying an operation now? The flapping bit of meniscus in on the way to detaching anyway.
Does the cleaning up of the meniscus after cutting away the damage – prevent further tears?
best wishes and thanks for your time
David (UK)
removing the offending flap is often enough to lead to improvement in your pain. You are still left with the majority of your meniscus, so, yes it can go on to tear again.
It sounds like it might be the appropriate course of action for you to pursue. There is always a risk of developing OA .. but that risk starts to increase once the meniscus tears. AS long as the resection or removal is not aggressive then the risk shouldn’t be higher than it already is.
Hi Dr Luks,
Im 50 years old. My pain in my right knee started 2 weeks ago. I went to a orthopedic surgeon and ask me to have MRI. The result of my MRI are as follows:
1. Horizontal tear, anterior horn of the medical meniscus
2. Bone bruise, patella and subcortical area of the medial tibial plateau,
3. Subcutaneous edema, anteroinferior aspect of the knee,
4. Suprapatellar joint effusion,
5. Popliteal cyst
I feel less pain now but i hear a popping sound when ever I climb the stair. Doctor told me I need a laser surgery. Do I have to see another doctor for a second opinion?
Thank you very much Dr. Luks and looking forward to your reply.
Do you think that you need surgery? Consider this a quality of life decision. Those “bone bruises” might be due to some arthritis. So there is no rush to consider anything.