
Indeed, a degenerative meniscus tear cannot be normal? Right? Hang on a moment. We will get to that. Many people with meniscus tears sit apprehensively in my office expecting to leave my office with a surgery date on their calendar. Instead, the majority of those patients will go home without the need for surgery, and without the need to dramatically alter their lifestyle. Why is that? Don’t we need surgery for a “tear”?
When the meniscus is healthy, it serves an essential function. When the meniscus is healthy, and not degenerative or worn out, it assists in a crucial role as a shock absorber. But the two menisci in our knee change and lose some of their function as we mature. It’s natural to think that a tear must imply that surgery is necessary. Give me a few minutes of your time to explain why an operation might not be your first choice to address your knee pain.
OUR JOINTS AGE TOO
Many of you reading this are older than 45 and do not recall a significant injury which led to your meniscus tear. Kneeling to pick something up or crouching to get something out from the freezer doesn’t count as an injury. Most of you had knee pain, saw your primary care doctor, or a specialist and were told that an MRI was necessary. You are shocked that your MRI shows a tear, and naturally, you expect to need surgery to fix this issue.
Read: Why an MRI isn’t always necessary.
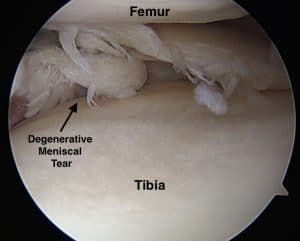
Most meniscus tears in middle age an beyond are “complex degenerative tears.” Think of your favorite pair of denim jeans. You didn’t tear your meniscus, just like you didn’t rip the front of the knee of your jeans. The tissue has started to fray, but the overall shape is maintained. That means no loose pieces are floating around and nothing is getting caught.

WHAT IS A DEGENERATIVE MENISCUS TEAR?
WHAT DOES THE CURRENT SCIENCE SAY?
The current research on this topic is evident. The majority of people with knee pain and degenerative meniscus tears have a great chance of responding to physical therapy alone. The majority of you will not require surgery. We remember in our youth that aches and pains subsided in days. Well, those days are long gone. Now it might take a few weeks for the pain from a meniscus tear to improve. So be sure to give it enough time before jumping onto to someone’s surgery schedule.
OSTEOARTHRITIS AND MENISCUS TEARS: A TRICKY COMBINATION

If you have osteoarthritis as well as a meniscus tear, then your chances of responding favorably to surgery diminish even further. Arthritis implies that you have lost the cartilage that covers the end of the bone. Once that cartilage is gone it cannot be regenerated. “Scraping” arthritis is not successful as alleviating the pain of arthritis. There are many people out there who regret having surgery for a degenerative meniscus tear. The operation, by removing a portion of the meniscus can start a chain reaction that leads to worsening arthritis. That might accelerate your trip to an operating room for a knee replacement surgery. And the research into how to treat people with mild arthritis and meniscus tears also shows that many will respond to physical therapy and the start of a resistance exercise program.
CAN I EXERCISE WITH A DEGENERATIVE MENISCUS TEAR?
Many of you can’t imagine how moving or exercising a knee with a tear and arthritis can be beneficial. That is intuitive. When we talk about your fears, many of you reveal that you are in my office because you want to be sure that you can go on with an active lifestyle, despite your meniscus tear. You’re afraid you might make things worse. The science in this area and 20 years of experience in this area supports maintaining an active lifestyle. The majority of you will feel better and not require surgery for your meniscus tear or your arthritis.
BUT I STILL HAVE KNEE PAIN
Yes, that brings up a very cogent point. You may still have some pain, despite physical therapy, weight loss, Tylenol and exercise. The proper question to ask yourself is whether or not the pain that you have now is tolerable or not. Is the pain severe enough to undertake the risks of surgery, and the possibility that your pain might worsen after surgery? You need to ask your surgeon if they expect your knee to be completely pain-free after surgery. Most of us will answer that honestly and will say it’s possible. You should ask if the operation could make the pain worse because the correct answer is yes. If you have arthritis, or thinning cartilage, then you may not be pain-free after surgery. It’s a toss-up.
Many surgeons might inform you that meniscus surgery will prevent arthritis from occurring. This statement is not accurate. Removal of a piece of meniscus puts you at a higher risk of developing osteoarthritis.
WILL THE TEAR BECOME LARGER IF I DON’T HAVE SURGERY
Will the tear become worse if I don’t have surgery? That is not likely, and certainly not a good reason to subject yourself to the risks of anesthesia, the risk of developing arthritis and the risk of feeling worse after surgery. If the pain that you are having is tolerable and does not interfere with your quality of life, then you may not want to consider an operation because you are afraid of something that may or may not happen in the future.
IS MENISCUS SURGERY AN OPTION?
Yes, some people might respond very well to meniscus surgery. While most of your knee pain might improve with time, PT, exercise, and over the counter medications, some of you will have severe persistent pain. As long as you do not have any significant arthritic changes, then surgery might be an appropriate option for you to consider. Your recovery might be straightforward, or could be rocky. This post discusses the recovery from meniscus surgery.
Additional Reading on Meniscal Tears:
- What is a Meniscus?
- Types of Meniscus Tears
- Why do meniscus tears hurt?
- Do all meniscus tears require surgery?
- Recovery from meniscus tear surgery.
nbsp;











Thank you for your website and responses! I’m finding it very helpful. I’m 58 and reasonably fit, until a month ago I routinely hiked 5-10 miles, lots of walking and yoga, plus occasional cycling, skiing, swimming, etc. One day I woke up (no injury I could recall) and could not walk more than a block without steadily increasing pain on the medial side of my knee. MRI showed medial degenerative tear and some evidence of arthritis. I was told surgery and “conservative treatment” were going to be equally effective, so I decided to avoid surgery. I was also told PT was unnecessary, was prescribed diclofenac for a couple weeks and told to wait 6-8 weeks with minimal walking (20 minutes max) and some adapted slow yoga. A month into this I can’t walk more than 10 minutes without the pain setting in. Should I be seeing more improvement by now? I’m thinking of getting a second opinion to see if there is anything I can do to improve my odds of recovery. Does this sound like it might be more of a surgical case? I don’t want to end up even worse but this is pretty discouraging. I had imagined retiring in a few years and traveling, hiking, walking! Not trying to climb Everest or run a marathon — just be active in the outdoors and enjoy life in a way that seems reasonable for a fit person my age. Not ready to give all that up.
HI Stephanie… PT can be effective.. but the type and tear and severity of the arthritic play a role in determining the best course of action. I couldn’t comment further about treatment options without seeing you.