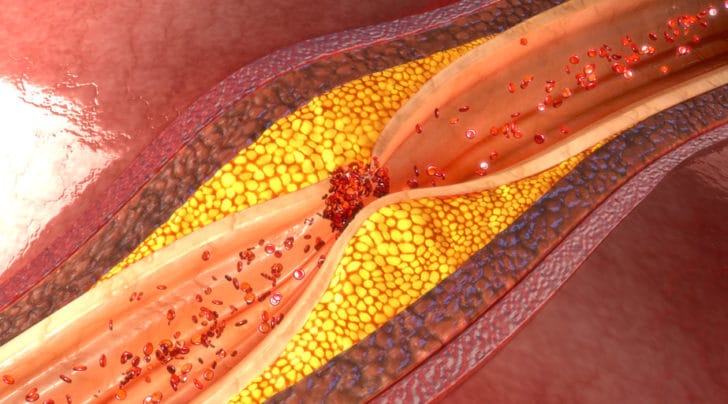
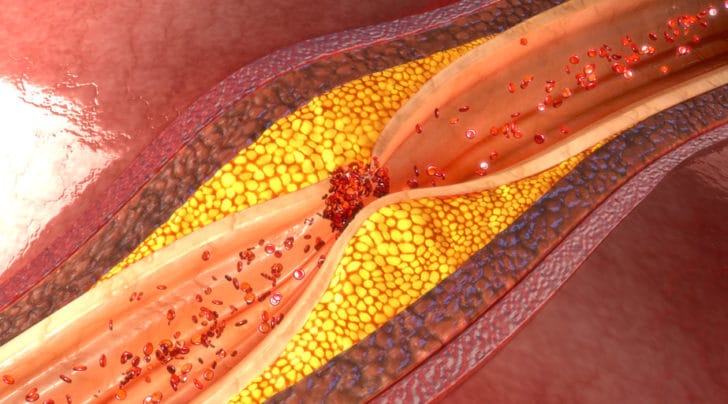
LDL and ApoB Exposure and the evolution of heart disease
Howard J. Luks, MD Updated Apr 30, 2022 Read time: 5 mins

Howard J. Luks, MD is a leading orthopedic surgeon & sports medicine specialist. An expert in shoulder, knee, and other sports injuries, and author of Longevity... Simplified.
Join the thousands of followers who rely on Dr. Howard J. Luks, a board-certified orthopedic surgeon specializing in Sports Medicine, with tools, tactics, and techniques for simplifying longevity.
Join the thousands of followers who rely on Dr. Howard J. Luks, a board-certified orthopedic surgeon specializing in Sports Medicine, with tools, tactics, and techniques for simplifying longevity.
An easy-to-read guide that tosses out the myths and clears up the truth behind living longer. As you read this book, you will: