Cartilage regeneration has been a focus of Orthopedic Surgeons for decades. Cartilage damage or defects can occur after an injury such as an ACL tear. Cartilage has proven to be a very difficult tissue to work with… and it has frustrated researchers, surgeons, and patients. The FDA recently approved a process in the US known as MACI. Autologous chondrocyte implantation has been around for decades. The name implies that we biopsy and grow your own cartilage, then at a second procedure implant the grown cartilage back into your knee. Discussed in detail below, MACI offers surgeons a potentially more reliable method to regenerate cartilage damage in your knee.
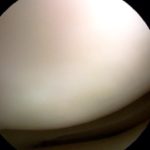
Cartilage is a firm, rubbery substance that is on the end of your bones. Cartilage enables our joints to move and glide without any friction or any pain.
Cartilage can be damaged from auto accidents, falls, sports injury or as part of a degenerative or arthritic process. If the cartilage is damaged then there is a hole or defect in the surface that normally protects the bones of the knee. Those holes or areas of damaged cartilage can spread and lead to osteoarthritis.
Cartilage Regeneration:
Over the years the Orthopedic industry has tried many different techniques to fill these holes in the cartilage. One of the most commonly performed procedures is a microfracture. That is a procedure where we make many holes in the bone. Those holes allow bone marrow cells to enter the knee joint. Those cells will form a layer over the area of damaged cartilage. The issue with a microfracture is that it didn’t work for everyone and the new cartilage was not as firm or as strong as the cartilage you were born with. That issue led to other techniques to try and repair a cartilage injury. You can review those techniques here.
A technique known as an ACI was popular a while back. During an ACI we grew your own cartilage cells then placed them under a patch we sewed over the hole in your cartilage. That technique was met with mixed results — although when it worked the new cartilage was firmer and stronger. Vericel, the company that invented the MACI process appears to have improved upon the results obtained with the ACI procedure. In addition, they have simplified the procedure.
MACI procedure for cartilage regeneration

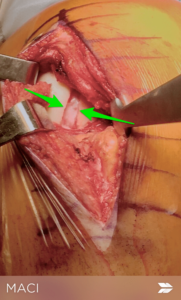
5-6 weeks is necessary to grow and implant the new cartilage cells onto the matrix. Then we bring you back to the operating room. This time we will make an incision in the front of your knee. The cartilage defect will be cleaned up and prepared. After proper preparation, we implant the new matrix with your cartilage cells into the defect. We attach the matrix to your knee with a biological glue or very small sutures.
Over the months after surgery, your cartilage cells will grow until the hole or defect in the damaged area of the knee is covered with new cartilage. The overall recovery is long and may require a period of time on crutches so you do not damage the new cells which they are growing. After a period of time on crutches, you will begin weight bearing exercises. The entire rehabilitation depends on the size of the defect or hole in the cartilage. The larger the hole, the longer the rehabilitation.
This paper shows that the MACI procedure appears to offer superior results when compared to a microfracture for cartilage regeneration. As with any relatively recent procedure, time will tell if the cartilage that grows is similar to the cartilage that you were born with. If the cartilage is of superior quality than MACI might offer Orthopedic Surgeons a new method to regenerate cartilage and minimize the risks of developing osteoarthritis.
You can read more about the MACI procedure here.












Dr. Luks,
Will this procedure work for patients with joint laxity or EDS – hypermobile type?
I don’t see why not. The key with proper patient selection for MACI is the type of cartilage defect. Traumatic cartilage defects are the best application of this technology. Trying to use this on degenerative or arthritic lesions is not likely to be met with success.
Hi, I had cartilage removed in 1974. I have a little left, but not much. Would this treatment help mwith? If so how can I find a surgeon in my area that performs the procedure?
It is not a technology which is useful in a degenerative or arthritic knee. It is primarily used for cartilage defects due to trauma.