The cost of surgical complications is extraordinarily high. We can look at this in two ways. The cost to the healthcare system and the cost to the patients. Both pay dearly for surgical complications that could have potentially been prevented.
The concept of value-based healthcare involves providing quality care at a lower cost. That sounds great. Who wouldn’t want to go to a hospital with a lower risk of complications? Many issues arise when discussing value-based initiatives, like who determines what “quality” is? Who decides what the penalties might be? Right now, these are very one-sided determinations. That has soured the widespread adoption of value-based initiatives for now.
There are hernia centers that can provide a hernia repair at a lower cost and lower risk than other hospitals. Some centers provided joint replacement surgery at a lower cost with a lower complication rate. Yet, those centers, under current value-based government programs, ended up losing money on all of their surgical cases. So this is an area that will require a lot more attention going forward if widespread adoption is the goal.
No one will argue that risk reduction strategies are critically important. No one will argue that complication rates should be as low as reasonably possible. Large self-insured companies will be pushing the value side equations more so than the government or private payors. In the end, the pressure will come from all sides (employers, patients, and insurers) for doctors and hospitals to provide data that they are capable of minimizing the risk of harm to our patients while bending the cost curve in a favorable direction.
You have all heard the term value-based care. How the US system will transition from a purely fee for service system to a value-based system remains largely unknown. It’s impossible to debate the fact that we all want better care, lower cost, and at a lower risk of complications. How all sides will define and measure value is still up in the air.
Suffice it to say, providers who ignore the value-based changes that are emerging are at risk as we move forward. Minimizing the risk of surgical complications, especially those associated with modifiable risk factors, will be one of the hallmarks of a value-based system.
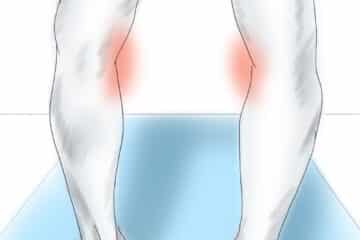
Joint replacement surgery has seen a significant rise in the total number of cases being performed. 600,000 knee replacements were performed in 2016. That is anticipated to grow to more than 3 million per year by 2025. The economic cost and patient suffering associated with complications from joint replacement surgery are enormous. There will be a lot of pressure moving forward for centers of excellence to emerge and prove that they can offer knee and hip replacement surgery at a lower cost and a lower risk of complications. We have the means to assess modifiable risk factors associated with higher rates of complications after joint replacement surgery.
Risk Factors for Knee Replacement Complications
Over the last decade, data has emerged on the risk factors that place patients at risk for developing complications related to poor preoperative optimization. Infections after a knee replacement are a life-altering complication. Attempting to eradicate an infected prosthesis is costly, fails often, and results in significant suffering for the patient, and a costly burden for hospitals, payors and all of us who ultimately pay more to care for these patients in the form of higher insurance premiums.
If 3 million people will be undergoing a knee replacement by 2025 and the risk of complications associated with modifiable risk factors is double that of a population at normal risk, then 30,000 patients per year or more may suffer needlessly. Employees lose money, mobility, incur significant expenses, and may lose their job or their home. Employers lose seasoned employees and pay a substantial price per episode of care. That price will be passed onto the rest of us as consumers downstream. The cost to the system will be tens of millions of dollars for the management of complications from knee replacements alone.
Complications due to joint replacement surgery will always occur
There are very few complications whose incidence can approach zero. The government and certain payors may consider infections to be never events, but the complexity of human biology will make achieving that impossibly difficult. Until Medicare and other government programs emerge to care for the elderly outside of the hospital, we will never be able to bend the cost and complication curves in the right direction. Food insecurity, housing insecurity, and around the clock care for the frailest among us will be essential considerations if fully encompassing risk reduction strategies are to be effective for our most at-risk patient populations.
Even without specific elder care initiatives, we can significantly diminish many complications associated with other known modifiable risk factors.
Those risk factors for perioperative infection risk include:
- nutritional status
- smoking
- glucose control
- weight
- medication adherence
- food insecurity, and
- housing insecurity
Infection risk after a knee replacement
Infections after a knee replacement are not common. Infection following a knee replacement, however, is a life-altering event. Most patients will go on to require two or more operations after the diagnosis of an infection is made. Despite those two operations, the risk of being re-infected approaches 20+%. It seems very logical that we do everything we can to try and control as many modifiable risk factors as possible prior to knee replacement surgery to minimize the risk of infections.
An important study in 2013 reviewed the results of 56,216 knee replacements. 63.0% were performed in women, the average age of the patients was 67.4 years, and the average body mass index (BMI) was 32 kg/m2. The incidence of deep surgical site infection was 0.72% (404/56,216).
Risk factors found to be associated with an increased risk of infection after knee replacement surgery include:
- BMI of ≥35
- diabetes mellitus
- an American Society of Anesthesiologists (ASA) score of ≥3
- Operative time was a risk factor, with a 9% increased risk per fifteen-minute increment.
- LINK TO THE ARTICLE
Modifiable risk factors to minimize the risk of complications following knee replacement surgery
Granted, we cannot control all the risk factors associated with surgery. Infections will always occur. The concept that health care providers and patients need to buy into is that controlling for modifiable risk factors is crucial to bring the risks associated with surgery as low as possible. Going forward, doctors and hospitals will be at risk for complications that occur. Our patients were always at risk and have always paid dearly for these complications.
The modifiable risk factors that have the most significant impact on the risk for infection and complications include.
1. Glucose control: Hyperglycemia and poor glucose control affects every system in our body. This is ultimately why people with diabetes are at higher risk for kidney failure, heart attacks, strokes, dementia, infection, cancer, neuropathy, and so on.
Advanced glycation endproducts (AGEs) occur when glucose or sugar interacts with other substances such as protein. These AGEs are “sticky.” They can “clog up” the metabolic machinery in our body and disrupt the normal function of organs such as the kidney. AGEs are a significant cause of many of the unfortunate effects that diabetes has on our longevity and healthspan. Hemoglobin A1c is a measure of an AGE that occurs in your blood in response to its exposure to glucose. An elevated hemoglobin A1c reveals poor glucose control over the long term.
Hyperglycemia suppresses our immune system. An A1c is of value as a screening tool, but there are better alternatives available. Tests such as a fasting insulin level will reveal issues with glucose metabolism long before the Hemoglobin A1c rises. Short term nutritional interventions can improve glucose control and decrease the risk of complications.
Hemoglobin A1c over 6.5 increases the risk of infection after knee replacement surgery. A blood glucose level > 200 at the time of surgery also increases the risk of infectious complications. Blood sugar must be considered from a short term and long term perspective.
Many surgeons and hospitals are starting to implement A1c levels above which your surgery will be delayed. This delay is in everyone’s best interest. Going forward, fasting insulin levels might prove to be a better marker in non-diabetic populations.
2. Smoking: Smokers have a higher risk of infection after knee replacement surgery. They have a higher risk of wound healing complications and thus have a higher risk of requiring another surgery to address wound issues or an infection after a knee replacement. A smoker should quit smoking for a minimum of two weeks prior to an elective knee replacement. Many providers will check serum levels of nicotine or cotinine the day of surgery to assure compliance with this request.
3.Nutrition: A standard American diet is a calorie-dense diet, yet often provides very little nutrition. There are a large number of malnourished obese patients out there. An albumin level below 3 predicts wound healing problems. You shouldn’t have surgery if you won’t be able to heal your wounds. That’s because you need protein to be able to heal your incisions.
Patients who are malnourished will also have lower immune system function. That means that your white blood cells, which fight infections, will not be working as well as they could be.
Deeper dives with pre-albumin and transferrin levels may be necessary too, but screening patients with an Albumin level will pick up most malnourished patients in our practices.
4.Weight: There are many reasons why obesity increases the risk of complications following a knee replacement. Your size affects the length of time it takes to perform a knee replacement. The risk of infection increases for every 15-minute block that the joint is open and exposed to the air.
The sizeable fatty layer under your skin presents a wound closure issue and may leave dead space, which collects blood and serves as a potential source of infection.
As mentioned, many obese patients are malnourished. That can affect healing, glucose homeostasis, and the nutritional status of the immune system. I’m often amazed at how poor your muscles look despite being hidden under 4 inches of fat and the fact that your muscles are subject to the large forces your weight brings to bear on them.
A BMI above 35 is often associated with type 2 diabetes. As mentioned, this compounds the issues associated with poor glucose regulation when present in the obese patient population.
In the long run, obesity also increases the risk of total knee replacement failure due to aseptic, or non-infectious loosening.
Risk levels increase for BMI > 35 and rise more dramatically for a BMI over 40.
5. Housing. It is essential to know where your patient will be going after the surgery. Skilled nursing facilities provide little value and are very costly. But we cannot send a frail patient who lives alone and has a two-level apartment home after surgery either. Working with these patients before surgery is important. Discharge planning should start well before the day of the procedure.
Assessing the risk of a knee replacement patient.
We have many tools available to us to determine if you are at an elevated risk of complications associated with your planned knee replacement. These tools have the advantage of offering us a chance to improve your risk profile before the day of surgery.
Preoperative Blood tests:
Routine blood tests should include a blood count (CBC), a hemoglobin A1c (or fasting insulin level), an albumin level, a vitamin D level, a basic metabolic panel, or BMP to assess your risk for metabolic syndrome and other issues that may affect your surgical risk profile.
Do you have questions regarding an Orthopedic injury or longevity?
Do you want to talk to an expert who can listen to you for 45-60 minutes and explain the options in detail?
Dr. Howard Luks offers remote guidance sessions to review your X-ray or MRI images and explain your options.
Dr. Luks has also received hundreds of requests for educational sessions on the topics discussed in his book, Longevity Simplified.
In addition to blood tests, there are other scoring systems utilized, which take into account your medical history, weight, and other variables.
ASA score:
Our anesthesia colleagues came up with what initially appears to be a very subjective assessment called the ASA Score. Despite being very subjective, it does help predict certain risk patterns associated with surgery.
The ASA score is a subjective assessment of a patient’s overall health that is based on five classes (1 to 5).
- Patient is a completely healthy fit patient.
- Patient has mild systemic disease.
- Patient has severe systemic disease that is not incapacitating.
- Patient has incapacitating disease that is a constant threat to life.
- A moribund patient who is not expected to live 24 hours with or without surgery.
NSQUIP:
The American College of Surgeons has a risk calculator referred to as NSQUIP. This is a tool that the surgeon can use to stratify the risks their patients will face. We input several known variables, and a risk score is determined.
Sleep apnea; Stop Bang score:
Sleep apnea is a common problem in our society. The risks of cardiac complications, such as a heart attack, are much higher in untreated sleep apnea patients. The Stop Band Score is a predictive tool to assess your patients’ risk of having undetected sleep apnea.
ERAS Protocols:
The idea behind ERAS was a reduction of postoperative physical and psychological stress, thereby decreasing recovery time and overall financial burden. These protocols initially focused on abdominal surgery, but have been adopted for joint replacement surgery as well.
ERAS protocols have been widely adopted and focus on preoperative variables as well as different forms of anesthesia and post-surgical management in order to enhance recovery after surgery.
When utilized, ERAS protocols can decrease the complications and costs associated with joint replacement surgery.
Weight/BMI:
If the BMI is greater than 35, then the risks associated with knee replacement start to increase. Above 40, they increase even more dramatically. The time to start the discussion with our patients about their weight is during their first visit when a diagnosis of osteoarthritis is made. If they understand that the day will come when their pain is terrible, yet we may not be able to perform their surgery because of their weight, perhaps that will provide the incentive necessary for them to adopt healthier eating patterns to bring their weight under a certain threshold.
This strategy has worked in our office. It is challenging, but it is a conversation that must start as early in the process as possible.
The value side is here to stay:
Value-based health care initiatives are not going away. Self-insured employers have already started to pursue them aggressively. And they should. In the not too distant future, we will need to provide data to insurers and the government to demonstrate that we are capable of providing surgical care at a lower cost and a lower risk of complications.
While insurers, employers, and the government are important players in this space, our patients and their health should be what matters most. Decreasing the risk of a life-altering complication such as an infection should be a goal we all wish to pursue for no other reason than to lessen the potential harm associated with the services we provide.