
If you are considering a total knee replacement you no doubt you are in significant pain, you likely have a significant disability and your quality of life is probably suffering as well. Nobody knows this better than you!
A total knee replacement is a BIG procedure… you must be well informed, and you MUST be *ready* for it. You should understand the procedure, the risks, the potential complications and the realistic goals! Once you understand that you can then make an informed decision whether or not you feel the “risk-benefit” ratio is in your favor.
Above all else… the decision to proceed with a Knee Replacement is a quality of life decision.
When all is said and done you have a 90+% chance of doing “well” and being pleased. But it will not be a quick and easy path.
Transcript:
Total Knee Replacements:
It dawned on me that I’ve been talking a lot about various issues we deal with in health care — effects of cost and how that affects everyone — overtreatment, overutilization — whether doctors should be involved in social media, etc., but I haven’t spoken much about medical topics. Let’s change that, shall we?
Let’s talk about knee replacements. This happened to have been a very busy week in the office with regards knee replacements. We saw a number of patients considering a knee replacement and we saw a number of knee replacements back in the office in follow-up and even saw some unfortunately in the emergency room.
Why do we do knee replacements?
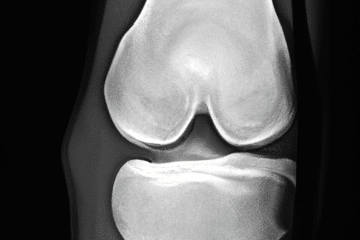
Knee replacement — the primary indication for knee replacements is arthritis — whether it is rheumatoid arthritis, osteoarthritis (which is the most common and usually genetic in origin) or posttraumatic arthritis (you had trauma previously or a fracture and the knee has gone on to degenerate) — what these all have in common is that you’ve lost the cartilage. You’ve lost the cushioning on the ends of the bones and now the bone ends are rubbing together. Does the mere fact that you have arthritis mean that you need a knee replacement? No. We don’t treat an x-ray. We don’t treat all MRI finding. We treat a patient. I’ve seen patients with horrible-looking x-rays and they are walking in with a cane, taking Tylenol and doing just fine. I’ve seen people with fairly mild to moderate disease but a have significant amount of inflammation and swelling with a profound corresponding disability. Now take that patient where they have significant pain and disability. They will typically say that the pain they are having is having a significant impact on the quality of life. The decision to go forward with a knee replacement is that you’ve exhausted all non-operative modalities or measures — medications, injections, therapy, etc. You’ve reached the point where you believe the pain is having such a significant impact on your quality of life that you’re willing to assume or perhaps deal with the risks associated with knee replacement.
How do we perform a knee replacement?
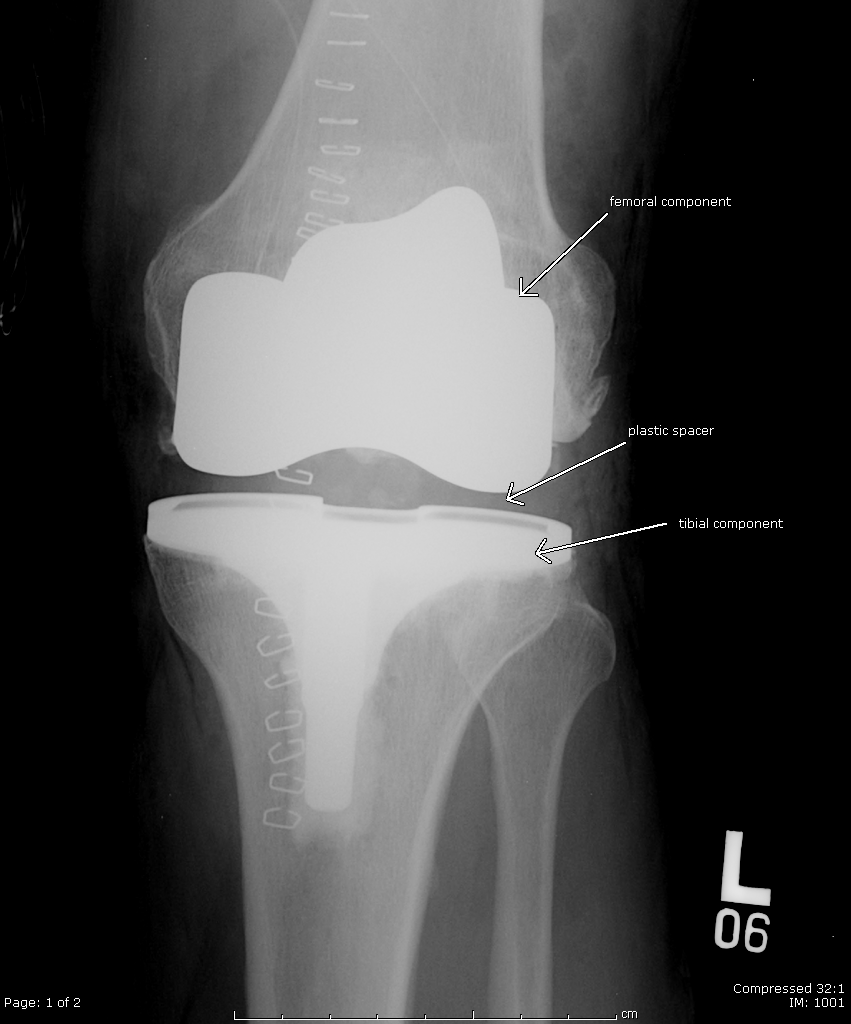
A lot of people think that we simply cut the ends of the femur, cut the top of the tibia and stick in this big, giant device. It’s not actually true. What we do is we actually reshape or resurface the ends of the bones. Here’s a knee, a simple knee. We have the femur on the top. We have the shinbone or tibia on the bottom. What we do is we remove a small portion of the end of the femur here, a small portion of the top of the tibia. This leaves us with the end of the femur cut and prepared for the prosthesis and the top of the tibia cut and prepared for the prosthesis. We then are able to put the prosthetic component on top of the bone like that. I’m obviously not a seasoned video personality. Then we put a tibial part in. We put a plastic spacer. We reduce the knee and that is a knee replacement. Notice how the replacement resurfaces the ends of the bone and that we haven’t actually cut across the end of the femur and taken the entire knee out.
Post knee replacement considerations
So you’ve decided that because of your pain, because of a significant impact on your quality of life, you’re considering a knee replacement. What are you looking at? You’re looking at a big procedure. No other way to put it. Some patients fly but the vast majority of patients experience significant pain and significant disability for a period of time and that period of time can be two to three months. What I typically tell people is that they won’t say “thank you” to me until around two months(after surgery). The procedure is successful in about 90-93% of people, that means that about 4 or 5% are going to have pain or some other issue with which you are dissatisfied. We don’t always know why. Their components look good on x-ray. They’re well fixed but the patient still reports some discomfort. One percent of you are going to be infected and a certain percentage may have a blood clot which will cause swelling in the leg and discomfort and so that leaves us with 92 to 93% overall success rate and when it goes well, it goes very well and people are very satisfied with their return to a mobile, active lifestyle with little, if any, discomfort.
Risks and some potential complications of a knee replacement
Are there risks involved with surgery? Absolutely. There is risk of anesthesia. The typical anesthesia for a knee replacement is spinal anesthesia. There’s risk of infection. The general quoted infection rate is about 1%. If you’re obese or if you’re diabetic or if you have a history of prior infections, the infection rate goes up from there. We give you antibiotics prior to the procedure. We wash the knee aggressively before we close the skin but infections still occur. Infections actually usually occur with your own bacteria so if you are having surgery it’s very important to shower very aggressively the night before and the day of the surgery to minimize the bacterial load on your body. What other risks are there? There’s risk of developing blood clots in the legs that’s called a deep vein thrombosis. That in and of itself is not dangerous unless the clot breaks off and travels to the lung. That is called a pulmonary embolus. That can be fatal. The incidence of DVT can be fairly high. However, the incidence of pulmonary embolus is very low and most surgeons, me included, put you on medications to dramatically minimize the risks of both DVT and pulmonary embolus. There is a theoretical risk of nerve or blood vessel injury. Those tend to occur in very deformed and posttraumatic stiff knees. The risk of nerve or vessel injury on routine knee replacement is very, very low. There is risk of issues with skin, with the incision not healing well and that is predominantly in diabetic or people with peripheral vascular disease. You could have issues with blood vessels also if you have a history of peripheral vascular disease. If you’re young, these components can wear out. They’re made of metal and plastic. If they wear out, they need to be done again. The components can loosen. With time your ligaments can stretch and if your ligaments stretched the knee can develop a feeling of instability and we may need to go back in and make that plastic piece a little thicker to re-tension or tighten those ligaments. Another common potential complication, is what we call patellofemoral instability – the kneecap sits on the front of the femur and that kneecap sometimes — will not ride in the center of a groove on the femur, as we want it to. Sometimes it slips over the edge and that leads to pain and instability and there are procedures to adjust that as well. Overall the complication rate of a knee replacement in general is 1-3% or less so again the vast majority of you do very well but ultimately remember it is your decision. No surgeon should tell you you must have a knee replacement. You should request a knee replacement after you failed nonoperative measures and you believe that your quality of life is so poor that it requires a knee replacement and you now are willing to assume the risks, some of which we just discussed.
Please remember… this is for informational purposes only and should not be considered medical advice. My online disclaimer applies.












Nice post. Simply the facts.
Verey informative-short and to the point! Thank you.
Thank you for your honesty and your generosity of your time to explain to all of us who are in need of a knee replacement. I have juvenile rhumatoid arthritis with both hips replacement and in need of new hips replacement in future months. My leg below my knee is crooked when I walk because of my bad knee. I will try to wait as long as I can but its getting really difficult to walk! Your knowledge as a surgeon will help me to decide for or against this surgery! Thank you!