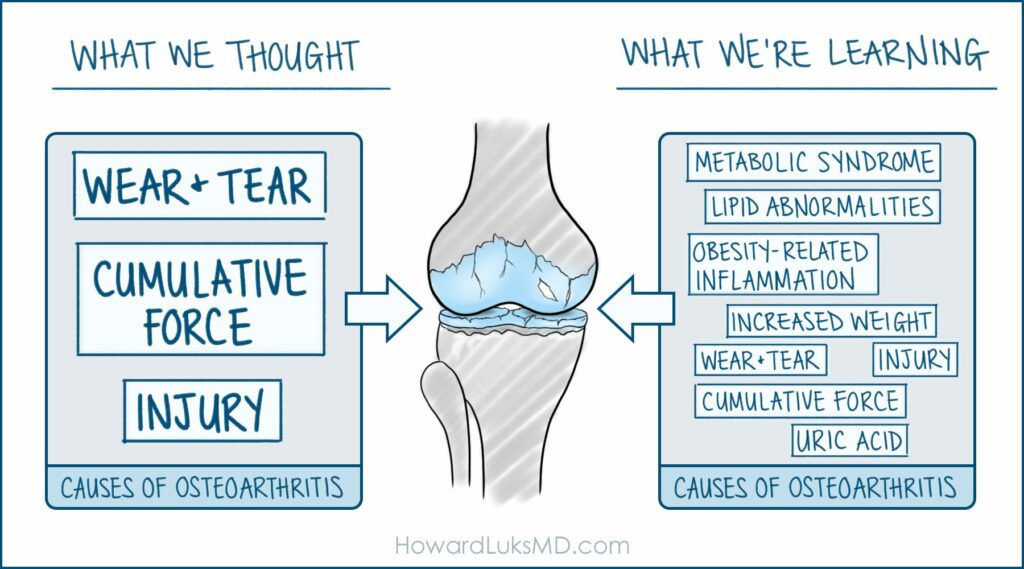
Osteoarthritis (OA) is the most common form of arthritis, affecting millions worldwide. Traditionally viewed as a wear-and-tear disease, recent advances in molecular biology have reshaped our understanding of OA. OA is a multifaceted disease involving intricate molecular pathways. This article delves into the molecular aspects of OA, focusing on the roles of inflammation, biomarkers, and genetic factors in its progression.
The Molecular Basis of Osteoarthritis
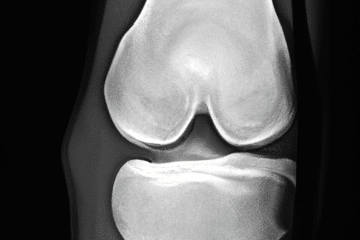
At its core, OA involves the breakdown of cartilage, the resilient and smooth tissue covering the ends of bones. However, this is not just mechanical wear but a dynamic process influenced by various molecular factors. These include:
- Inflammatory Cytokines: Cytokines are small proteins crucial in cell signaling. In OA, pro-inflammatory cytokines like Interleukin-1β (IL-1β) and Tumor Necrosis Factor α (TNF-α) are upregulated. They play a pivotal role in cartilage destruction by stimulating the production of enzymes that degrade cartilage components.
- Matrix Metalloproteinases (MMPs): These enzymes are responsible for the breakdown of extracellular matrix components in the cartilage. MMPs, particularly MMP-13, are often found in increased levels in OA and are a primary factor in cartilage degradation.
- Advanced Glycation End Products (AGEs): AGEs accumulate in cartilage as we age. They exacerbate oxidative stress and inflammation, contributing to cartilage degradation.
The Inflammatory Pathway in OA
Inflammation is now recognized as a critical driver of OA progression. Unlike rheumatoid arthritis, inflammation in OA can be more subtle, and chronic. Synovial (lining of the joint) inflammation leads to joint swelling and pain and significantly predicts disease progression. The molecular mechanisms of inflammation in OA include:
- Activation of NF-kB Pathway: This pathway plays a central role in the inflammatory response in OA. It regulates the expression of genes involved in immune and inflammatory responses.
- Synovial Activation: The synovium, the membrane lining the joint, becomes inflamed and thickened in OA. This synovitis is often associated with increased production of cytokines and other inflammatory mediators. This is also associated with a change within the cells in the synovium. They ‘polarize’ or change from an anti-inflammatory, reparative subtype to a hostile and destructive subtype.
Biomarkers in Osteoarthritis
Biomarkers are measurable indicators of a biological state or condition. In OA, they hold the promise of early diagnosis, prognosis, and monitoring of disease progression. Some key biomarkers include:
- Cartilage Oligomeric Matrix Protein (COMP): Elevated levels of COMP in the blood are associated with cartilage breakdown and can be an indicator of OA progression.
- Urinary C-Telopeptide of Type II Collagen (uCTX-II): This marker reflects the turnover of type II collagen, a primary component of cartilage. Elevated levels are associated with the severity of OA.
Genetics and Osteoarthritis
OA is a complex trait with both genetic and environmental factors. Several genes have been associated with an increased risk of OA, including:
- GDF5 (Growth Differentiation Factor 5): Variants in this gene have been linked to joint formation and are associated with OA susceptibility.
- FRZB (Frizzled-Related Protein): This gene is involved in the Wnt signaling pathway, crucial for joint development and homeostasis. Variants in FRZB have been linked to hip OA.
The Future of Molecular Therapeutics in OA
The growing understanding of the molecular underpinnings of OA paves the way for targeted therapies. Potential future treatments include:
- Biological Agents: These are drugs targeting specific molecules involved in OA. For example, inhibitors targeting inflammatory cytokines like IL-1β could slow down cartilage degradation.
- Gene Therapy: This involves introducing genetic material into cells to compensate for abnormal genes or to make a beneficial protein. Gene therapy could potentially be used to modify the expression of genes involved in cartilage degradation.
The molecular understanding of osteoarthritis has dramatically evolved, shifting the perception of OA from a mechanical to a biologically driven disease. This shift opens new avenues for diagnosis, treatment, and even prevention. By targeting the molecular pathways involved in the disease process, it may be possible to develop more effective and personalized treatments for OA. As research continues to unfold the molecular intricacies of OA, hope rises for millions suffering from this debilitating condition, marking a new era in the management of osteoarthritis.
Do you have questions regarding an Orthopedic injury or longevity?
Do you want to talk to an expert who can listen to you for 45-60 minutes and explain the options in detail?
Dr. Howard Luks offers remote guidance sessions to review your X-ray or MRI images and explain your options.
Dr. Luks has also received hundreds of requests for educational sessions on the topics discussed in his book, Longevity Simplified.