Should everyone be wearing masks to combat the spread of the COVID19 pandemic due to SARS-CoV-2?
Many people remain very confused as to whether or not they should be wearing a mask to minimize the risk of catching the novel coronavirus, SARS-CoV-2. That’s because there are dramatically different mixed messages emerging from all corners of the globe.
The World Health Organization, as well as the Centers for Disease Control, continue to suggest that mask-wearing out in the public space is not necessary. The CDC now recommends a “cloth face covering” should be worn. The White House refuses to recommend the routine wearing of a face mask while in public… thus the toned-down message from the CDC.
On April 2, 2020, the latest “rapid expert consultation” provided to the White House Office of Science and Technology Policy suggested that there was not yet enough evidence to confirm that masks should be worn in public. But these statements are worded carefully… they said not yet “enough” evidence.
Enough about politics … does the scientific literature suggest about wearing masks in public?
How do respiratory viruses spread from person to person?
Respiratory viruses are viruses that enter our body through the nose or mouth, progress down to the lungs and cause a lower respiratory infection. There are direct and indirect modes of transmission for respiratory viruses.
Respiratory viruses all have common, but occasionally different modes of transmission. That means that they can have different means of spreading from one person to the next.
Droplet transmission is the most common. “Respiratory” particles are different than droplets. A good example of droplet spread would be the reason why you have to clean your computer screen fairly often. You can see those not so tiny drops that are dried on your screen because of your presence in front of the screen over time. Imagine if all those droplets had millions of virus particles in each tiny circle ???
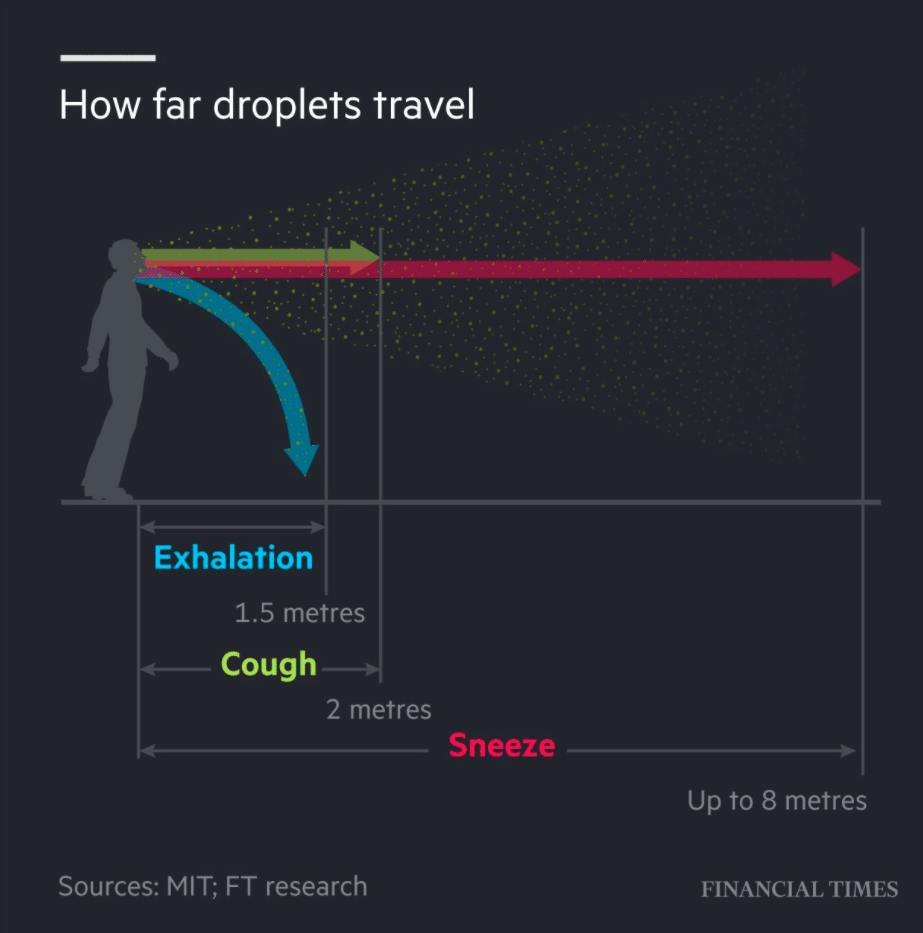
When people cough, sneeze or talk, most of those droplet particles will fall to the ground within a few feet of exiting your mouth or nose due to gravity. Some droplets will continue to linger in the air longer and travel further. Those droplets that can spread further are called droplet “nuclei”. They dry out soon after leaving the host’s mouth or nose. They are super small and can stay suspended in the air. This paper discusses the concept of droplet spread in more detail.
It has been very well established that droplet transmission is a common mode of viral disease transmission in general. Not only because the droplets can be inhaled through your nose or mouth but because those particles will land on the surface. The virus can stay alive within those droplets for up to a few days. Then, you come around and touch one of those droplets and then later that day touch your nose to wipe your eye and you now have millions of virus particles with a clear entry into your body.
Viruses that spread by “indirect respiratory” transmission do not require a droplet of saliva. Measles and chickenpox viruses are 2 classic examples of viruses that can spread by aerosol transmission. That means that the virus particle itself can remain suspended and there for hours. A virus particle is very small, so it can stay suspended in the air much longer. That’s why measles and chickenpox are very highly contagious and easy to catch. You could go into an elevator that someone with measles used hours ago and become infected. It is much more challenging to prevent infections by viruses that spread through a respiratory aerosol mode of transmission.
Is there enough evidence to suggest we should be wearing masks to limit the transmission of COVID19?
So, is there evidence to suggest that aerosol respiratory transmission of SARS-CoV-2 occurs in addition to droplet spread? Meaning… can you catch COVID19 from talking to someone who is infected but not coughing or sneezing? in other words, does an infected person leave viral particles floating in the air from just exhaling? Are those viral particles capable of causing an infection?
Maybe… it sure does seem like it does.
Researchers from the National Institutes of Health, Centers for Disease Control and Prevention, UCLA and Princeton University examined how long COVID-19 survives in the air as well as on copper, cardboard, plastic and stainless steel and then compared it with SARS.
Those researchers found that COVID-19 was detectable in the air for up to three hours. In addition, they found that COVID19 was detectable for up to four hours on copper and up to 24 hours on cardboard. SARS-CoV-2 can also last up to three days on plastic and stainless steel. It should be clear… just because the researchers find viral particles does not mean that those particles are capable of causing an infection. Many things can render a viral particle incapable of causing disease.
The research into previous coronavirus infections such as SARS and MERS combined with the “pre-print” literature emerging on COVID19 reveals that we should probably be considering wearing masks at all times while on the public space.
It should be made clear that there are no studies that absolutely support aerosolized respiratory transmission of SARS-CoV-2 without the presence of respiratory droplets.
OK, what we do know…
Very recent studies support that aerosol transmission is likely quite common with COVID19. The researchers found that the SARS-CoV-2 virus actively replicates in the upper respiratory tract (the back of your throat).
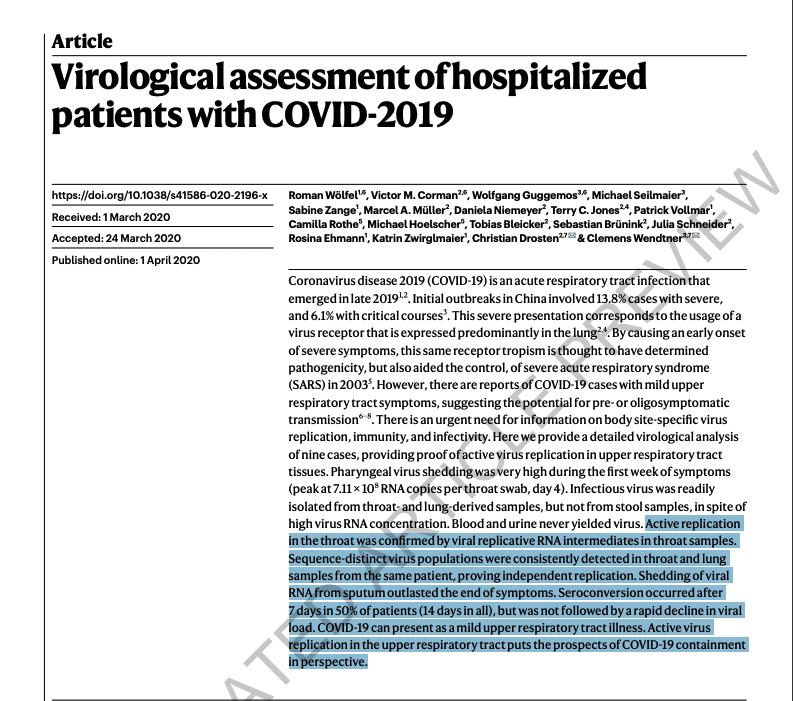
Many other respiratory viruses are found in the throat region, but they got to the throat only after actively replicating in the lung. That means that the virus was not actually replicating in the throat, but instead, the virus spread to the throat after being produced in the lung. Finding live, replicating, infectious virus in the throat seems to suggest that aerosol transmission of the novel coronavirus is possible.
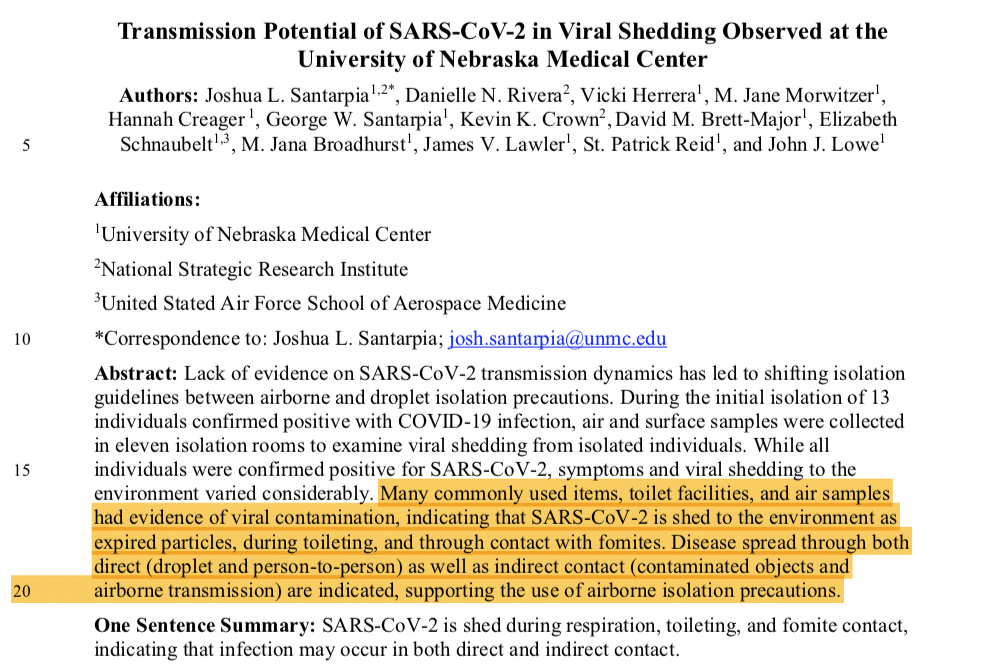
Another recent publication from the University of Nebraska revealed the presence of viral particles quite distant from known patients — who were not observed to be coughing or sneezing. These viral particles were found in the bathroom, on their cell phones, more than 6 feet away from their beds, and even in the hallways outside the rooms. But, this paper did not prove that these viral particles were capable of being infectious. That’s a very important missing piece of information.
Should everyone be wearing masks to prevent SARS-CoV-2 transmission?
While recent research has shown that the novel coronavirus can be identified in the air, researchers have not confirmed that those viral particles are infectious or capable of causing a COVID19 infection. That’s important… and that’s a critical missing piece. If it is proven that aerosolized viral SARS-CoV-2 particles can cause COVID19 infection then the WHO, CDC etc will all conclude that everyone should be wearing masks at all times. But, we are not there yet…
So… where are we?
We must protect our frontlines.
Our frontline emergency responders, as well as the frontline healthcare staff require the best possible precautions necessary to minimize the risk of getting sick. It is very clear that for aerosol-generating procedures, an N95 filtering respirator is necessary. Otherwise, all hospital workforce members should be wearing a surgical or procedure mask at all times.
Perhaps to make up for the lack of adequate levels of personal protection equipment and very poor government preparation, just last week the CDC allowed for the use of standard procedure masks instead of N95 respirators for aerosol-generating procedures in the hospital. That is irresponsible and endangers the health of our healthcare workforce.
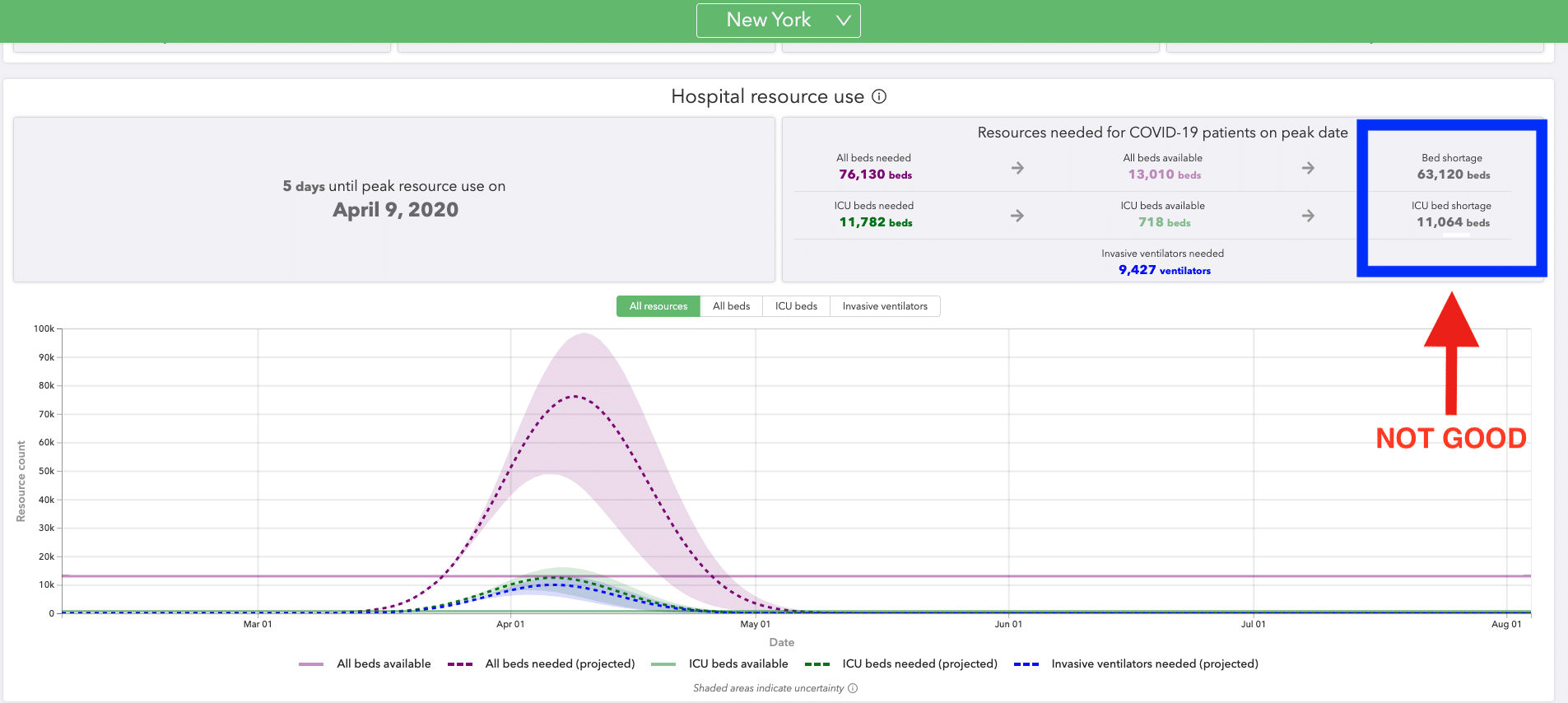
The graph above shows just how critical this situation is in NYC. This will play out in a similar manner in other cities across our nation over the next month. We need to do anything we can to decrease the spread of SARS-CoV-2. Many of those measures will be familiar. You’ve heard them before. But they all bear repeating.
How do we further minimize the risk of becoming sick due to COVID19?
- Continue with strict social isolation measures.
- Do not touch your face… ever. This is hard. Practice, practice, practice.
- Wash your hands often.
- Carry hand sanitizer with you. If you touch an object in public, sanitize your hands.
- Wear a mask, DIY or otherwise whenever you are out in public.
- Consider wearing glasses, goggles or a face shield. This virus can infect us by entering our bodies through our eyes.
- Don’t leave your home if you are sick.
- Clean your phones… don’t use your phones out in public unless it is an emergency.
- If you are sick, you must isolate yourself in your home. Separate bedrooms, and if possible, a separate bathroom. Clean the bathroom very well.
- Don’t be overconfident because you have a mask. You should still stay home and practice social distancing.
Until we have firm data the key strategy for minimizing the risk of COVID19 disease transmission outside the hospital remains following well-established social distancing measures. Our initial collaborative post from 10 days ago remains as relevant as ever. Feel free to share it with anyone who is still on the fence.
Do you have questions regarding an Orthopedic injury or longevity?
Do you want to talk to an expert who can listen to you for 45-60 minutes and explain the options in detail?
Dr. Howard Luks offers remote guidance sessions to review your X-ray or MRI images and explain your options.
Dr. Luks has also received hundreds of requests for educational sessions on the topics discussed in his book, Longevity Simplified.
Should we be using masks in public at all times?
It is not yet clear whether aerosol-based respiratory spread is a common mode of transmission for the novel coronavirus, SARS-CoV-2.
We do not have conclusive evidence that SARS-CoV-2 spreads via aerosol or indirect respiratory transmission. What we do have is mounting evidence which shows that this clearly could be a means of transmission from asymptomatic or minimally symptomatic people in the public space to others.
We also have proof that our healthcare system is not capable of handling the current number of COVID19 patients. And we are still 1-2 weeks away from the start of the surge in the NY region!!
Therefore, given the current evidence, as well as the mounting stress on our healthcare system I believe it is safe and prudent to suggest that everyone should be wearing a mask at all times when they venture outside their home and anticipate interacting with others in a public space.
When it comes to which masks should be worn this is very much open for discussion and deliberation. Clearly N95 masks are superior, however, these are needed by front-line workers and healthcare workers and should not be given to the public until the needs of the frontline workers have been met.
Many people are finding it hard to purchase masks. The DIY community has stepped up. Sewing instructions are easily found on YouTube, etc. This article claims that blue shop towels are a good material to consider lining your cloth masks with. Surgical procedure masks and even some homemade masks, particularly those made with blue shop towels appear to show that they offer a fair degree of protection.
Any mask appears better than no mask. No mask is perfect. No mask can prevent all infections. It is very important that you know how to take masks off properly to minimize the risk of infecting yourself.
I put this video up on Facebook to demonstrate how to remove a mask safely.
Disclaimer: I do not speak for my employer.
This is NOT medical advice. This is for informational purposes only.
Use a mask at your own risk.
Masks do not prevent all infections.
Wash your hands… a lot!