
Nearly 50% of Americans have Insulin Resistance (IR). People with IR do not have a typical appearance. Some of you with insulin resistance are thin and “healthy”. The presence of insulin resistance associates with many severe chronic diseases. How do we know if you have it.. and how is IR treated?
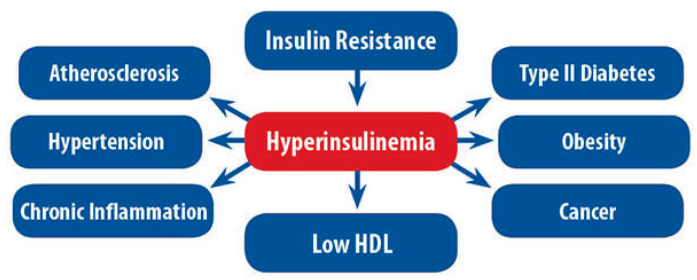
Insulin resistance can directly cause many diseases that lead to a shorter lifespan. In addition, insulin resistance can accelerate or worsen chronic diseases which are the most common causes of death. Insulin resistance will accelerate atherosclerosis, thus worsen the disease course of heart disease, hypertension, dementia, and stroke.
Because insulin resistance is so prevalent, we need to have a better understanding of:
- what is insulin resistance
- what drives IR
- what are the downstream effects
- how do we treat it?

I have been an Orthopedic Surgeon for nearly 25 years. While I have returned many athletes to the playing field with my knife and replaced more knee than I can count, but I am often most pleased by being able to dramatically help entire families improve their health with lifestyle and dietary modification. Those are, by far the biggest success stories in my practice. Returning people to a path of being metabolically healthy will impact their entire life and the lives of those they bring along on their journey.
Contrary to popular belief among some of my peers, people will often engage if they understand why they should and how to accomplish it. Over the last decade, I have chosen to optimize my own overall health and the overall health of those I treat. What often becomes evident in my interactions with you is that most of you actually do want to change your diets (within reason) and do want to exercise more. No one wants to continue their march down a path towards heart disease, stroke, or neurocognitive decline and disability. Information is empowering. Knowing why we need to change and how our actions can affect that change is very powerful and often very motivating.
What are insulin resistance and hyperinsulinemia?
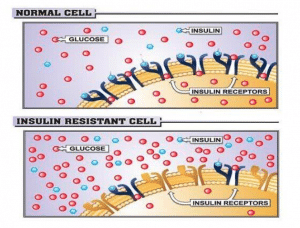
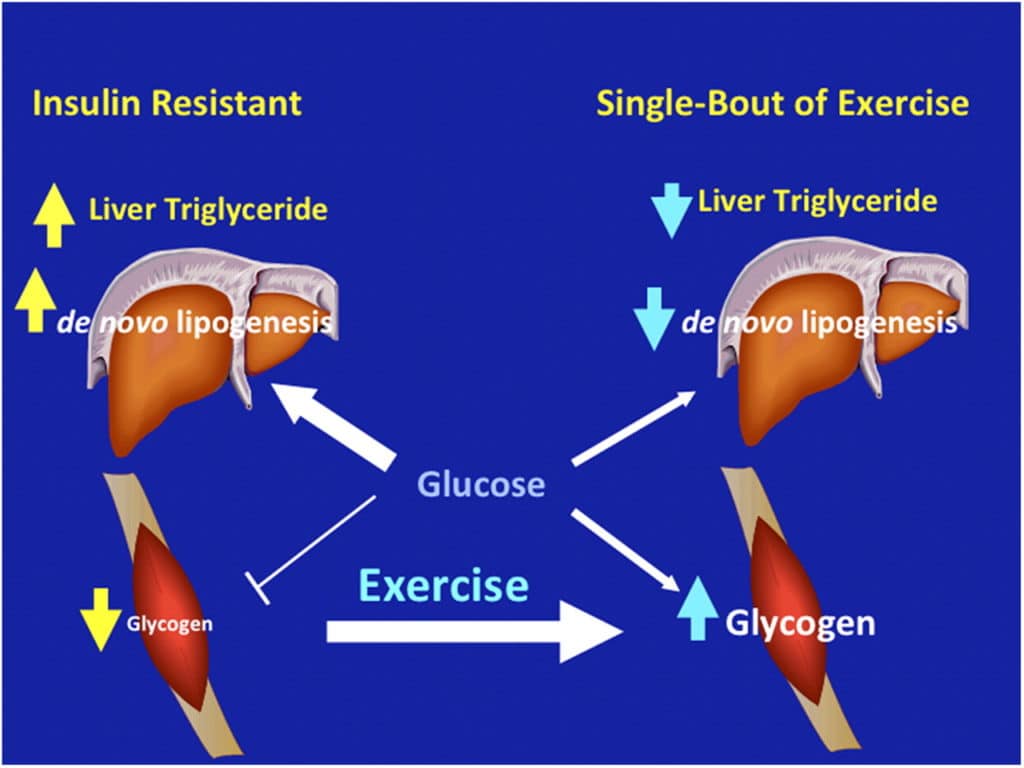
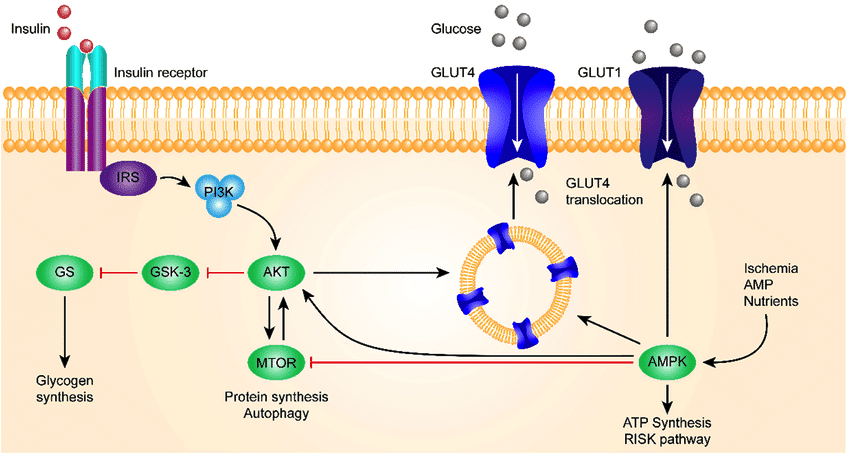
Yes, muscles can take some glucose in without insulin, but that occurs during exercise. If you are starting to require more insulin in your body to accomplish the same amount of glucose uptake into your cells then you have insulin resistance. If you have insulin resistant tissues, then your pancreas will need to make more insulin to maintain the same glucose levels in your blood. That is what we refer to as hyperinsulinemia.
Because of the increased insulin, your blood glucose level might look normal on routine blood tests. Your A1c levels will often be in the normal range. Your fasted insulin levels might look normal too. This is why your usual blood tests might not reveal the presence of insulin resistance for a decade or more.
Why are insulin resistance and hyperinsulinemia bad for your health?
Identifying people with high amounts of insulin in their blood and tissues that are resistant to the effects of insulin is very important. This should be called the pre-pre type2 diabetes stage. That means that you may not have hyperglycemia or high glucose levels yet. It also means that your hemoglobin A1c is still in a normal range. THIS is the stage that you want to intervene and help people become more metabolically fit. Why? Because your pancreas has beta cells. Those beta cells make insulin. After years of churning out too much insulin, they may grow tired and worn out. Once those beta cells stop working they may never come back. That is why some people with Type 2 Diabetes require insulin injections.
Hyperinsulinemia also causes your kidneys to retain sodium. That means you need to keep more fluid in your blood to dilute the sodium. That is but one reason why you have hypertension. In addition, hyperinsulinemia is associated with metabolic syndrome: hypertension, obesity, abnormal lipids, and glucose intolerance. Many diseases that are commonly associated with insulin resistance, such as fatty liver disease, elevated chronic inflammation, etc also lead to hypertension by stiffening the walls of your blood vessels. Imagine have a syringe full of water. You are asked to push that water through a soft, thin flexible tube with the syringe. As you push the syringe, the tube expands and allows the water to go through easily. Now, try to push that same amount of water through a stiff tube with a thicker lining. It will be harder to do it. The pressure in the tube will be higher. This is one reason you have hypertension, and why your heart is working harder.
Gerald I. Shulman
Proceedings of the National Academy of Sciences Aug 2011, 108 (33) 13705-13709; DOI: 10.1073/pnas.1110105108
Your Triglyceride/HDL ratio and what it tells you
- This ratio works best if your BMI is + or > 25 kg/m2.
- The African American population tends to have lower Trig levels. Therefore, different screening tools are needed (Oral OGTT). A normal Trig/HDL ratio does not rule out insulin resistance in African Americans.
Oral glucose tolerance tests (OGTT) can help diagnose insulin resistance.
An OGTT or oral glucose tolerance test remains the current gold standard to diagnose insulin resistance or hyperinsulinemia. During that test, we give you a drink with 75 grams of glucose. Then we check your glucose and insulin levels at 30-minute intervals afterward. Many people who have an OGTT will be shown to have insulin resistance. Their glucose will be elevated above what it should be, and more importantly, the amount of insulin in your blood needed to decrease that glucose level by driving the glucose into your muscle and liver will be increased.
Do you have questions regarding an Orthopedic injury or longevity?
Do you want to talk to an expert who can listen to you for 45-60 minutes and explain the options in detail?
Dr. Howard Luks offers remote guidance sessions to review your X-ray or MRI images and explain your options.
Dr. Luks has also received hundreds of requests for educational sessions on the topics discussed in his book, Longevity Simplified.
Researchers at Yale have found evidence of insulin resistance in 30-40% of thin, healthy appearing college student volunteers when subjected to an OGTT.
Ok… let’s keep going. Let’s say you haven’t had an OGTT.
Now we are going to discuss:
- Why the Triglyceride/HDL ratio helps predict risk… and once you understand that,
- What you can do to improve that ratio and decrease your odds of living with diseases associated with insulin resistance and hyperinsulinemia.
Sugar (glucose) and its effect on your triglyceride levels
 Lipids (fats) and sugar don’t mix … and this association is not logical to many of you. You’re not alone. This is not an intuitive issue for many people. Most of you associate triglycerides with fat. That is far more logical. Most do not understand that quite often there is a direct relationship between carbohydrate or glucose and your triglyceride levels. Therefore, let’s review a little basic physiology and show you how sugar increases your triglyceride levels.
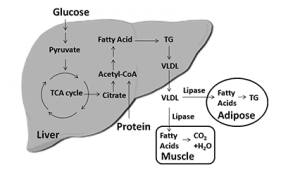
Lipids (fats) and sugar don’t mix … and this association is not logical to many of you. You’re not alone. This is not an intuitive issue for many people. Most of you associate triglycerides with fat. That is far more logical. Most do not understand that quite often there is a direct relationship between carbohydrate or glucose and your triglyceride levels. Therefore, let’s review a little basic physiology and show you how sugar increases your triglyceride levels.- Use glucose as energy.
- Store the glucose internally as glycogen (after exercise, or a period of fasting).
- Convert the glucose to triglycerides, package them into a VLDL particle, and send it out in the bloodstream for other tissues to use.
- Convert the glucose to fat and store it internally.
VLDL stands for very-low-density lipoprotein. Your liver makes VLDL particles and releases them into your bloodstream. The VLDL particles mainly carry triglycerides to your tissues. VLDL is similar to LDL cholesterol, but LDL particles mainly carry cholesterol to your tissues instead of triglycerides
When the VLDL particle containing the triglycerides gets into the blood, it can release the triglycerides at various target tissues:
- Trigs can be taken up by muscle and stored as intramuscular triglyceride for energy storage.
- Trigs can be taken up by muscle, broken down via a process called lipolysis, and used for current energy needs.
- Trigs can be taken up by the fat cells (adipose tissue) and stored in your adipose tissue for later use.












John Sainz
Thanks for the information Dr. Luks. Gonna get myself going here.. have to schedule a physical, after I find a good doctor. Know any good primary doctor in Putnam or dutchess counties?
Deepa
Hello,
Thank you for the Informative article. One question:why is it that only excess carbs consumption are what causes high triglyceride? Wont high fat intake also cause high triglycerides as these fattyacids can also easily be converted to TG.
Hi… There are many other causes of elevated triglycerides… I was highlighting one common association.
High triglycerides are usually caused by other conditions, such as:
Obesity.
Poorly controlled diabetes.
An underactive thyroid (hypothyroidism).
Kidney disease.
Regularly eating more calories than you burn.
Drinking a lot of alcohol.
Certain medicines may also raise triglycerides. These medicines include:
Tamoxifen.
Steroids.
Beta-blockers.
Diuretics.
Estrogen.
Birth control pills.
In a few cases, high triglycerides also can run in families. Thanks for your question!
Elena
Dr Luks,
Firstly thank you! You are just brilliant I love your information it certainly will change my way of eating carbs. I don’t have many however I do love roast potatoes occasionally :) I do take great care of myself I will take extra care after reading all your posts. No Doctor I know has ever taught me this much. I will tell them to look you up so they can learn how good you are. 😊🙏🏻🌈🇦🇺
Kind Regards
Elena