
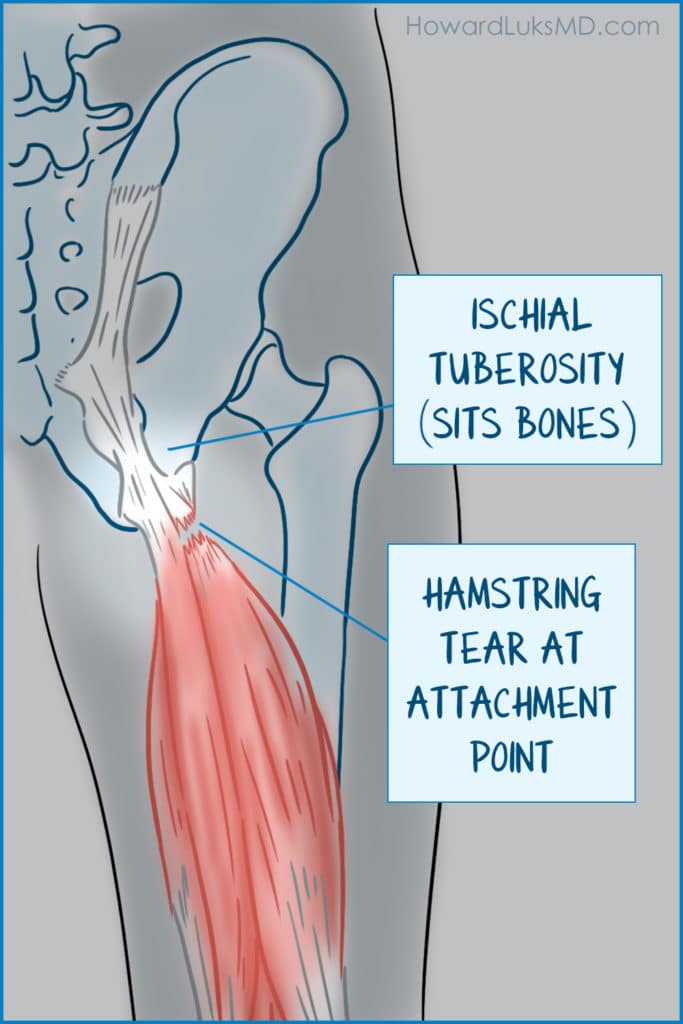
The hamstrings are a powerful group of muscles. They are subject to significant forces with sprinting, hill, and quick starts. There are three hamstring tendons that coalesce and insert or attach to the bottom of your pelvis at the “sits” bone– or the ischial tuberosity. That group of tendons can tear or avulse from the bone. Previously, most all proximal hamstring ruptures were treated surgically, but new data suggests that might not be necessary.
Surgical vs. non-surgical treatment of proximal hamstring tears.
In a recent study published in the British Journal of Medicine, a research group from the Netherlands looked at 50+ patients who had sustained a rupture or tear of the proximal hamstrings.
This was not a randomized controlled study. They used a shared decision-making process to determine who would have surgery and who wouldn’t. That essentially means that the authors shared the currently available data with the patients. They shared the risks of surgical vs non-surgical management and the patients decided which option they would pursue.
The group which choose to have surgery had a lower PHAT score prior to surgery. The PHAT score correlates complaints and symptoms and gives it a numerical value.
The authors found no significant difference between those who had surgery and those who did not. Both groups experienced a significant improvement in their follow-up clinical scores and their functional scores.
Well, should I have surgery for a proximal hamstring tear?
Couple of things to keep in mind. First, this was not a randomized trial. This was a shared decision-making trial. That makes it more difficult to compare apples to apples. Second, patients in the surgery group had lower PHAT scores. That could influence the results since people with more pain, and a greater sense of disability are more likely to choose surgery as an option. Third, the median ages were 49-51. So this might not be relevant to high-level younger athletes– we don’t know how they would do with non-surgical management.
This is an interesting paper and deserves our attention. It will not be the last word and should not set treatment precedent for proximal hamstring tendon tears. Further study is needed. Those studies could be randomized controlled trials or sham surgery trials. Furthermore, a better understanding of the patient-specific variables and how it influences their PHAT would be useful. Eg. Are they runners, athletes, sedentary, etc.
Do you have questions regarding an Orthopedic injury or longevity?
Do you want to talk to an expert who can listen to you for 45-60 minutes and explain the options in detail?
Dr. Howard Luks offers remote guidance sessions to review your X-ray or MRI images and explain your options.
Dr. Luks has also received hundreds of requests for educational sessions on the topics discussed in his book, Longevity Simplified.
But for now, this paper informs us that we need to discuss non-operative treatment of proximal hamstring tears as a non-inferior option for those who seek our opinion.












