Chondromalacia patella is a very common condition and is thought to be a common cause of anterior knee pain. It is more common in young women. “Anterior knee pain” means pain in the front of the knee. The term chondromalacia implies cartilage softening and thinning is taking place. Pain from chondromalacia will often present with burning pain in the front of the knee joint. Grinding or clicking in the front of the knee is also a common complaint. This condition is thought to be a common cause of anterior knee pain in runners, young women, and older adults when arthritis becomes more prevalent. We have a very popular, newer post on anterior knee pain here.
What is Chondromalacia?
Chondromalacia, very simply put represents a softening and possibly early degeneration of the cartilage underneath your kneecap or patella. It is more common in women, some as young as teenagers.
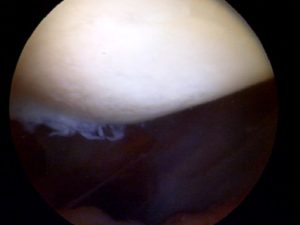
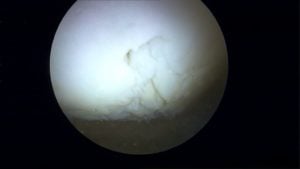
Cartilage is a very important structure in our knee. It coats the ends of all the bones in our knee which touch – or articulate- on one another. Healthy cartilage allows for motion without friction, pain, clicking or discomfort. Normal cartilage in our knee is usually quite firm and smooth with no divots, fissures or roughness. When chondromalacia sets in, the cartilage surface starts to soften. In time (years) the cartilage begins to develop fissures, torn flaps and becomes thinner than usual. If the cartilage begins to degenerate or change then your knee might hurt, it might click and some patients with chondromalacia or cartilage changes might have a feeling of “catching” or giving way.
Most people with knee pain due to cartilage issues experience difficulties or pain when arising from a seated position, or when climbing or going downstairs. Chondromalacia is not the only cause of anterior knee pain or pain in the front of your knee. This post explores the most common causes of anterior knee pain.
The exact cause of this condition is unknown. In many people, the cartilage on the patella or kneecap simply begins to change. This happens at the microscopic level. The supportive proteins and chemicals inside the cartilage start to change. We are not sure why that happens. Potential causes of chondromalacia include genetics, prior trauma, repetitive stress (a very common condition in runners) … or in the majority of cases we’re not sure why it has occurred. I have seen entire families with this condition in exactly the same area under the patella… supporting the genetic cause. Yet, I have seen some patients with extended families, no history of trauma, and they are the only ones who have severe chondromalacia. Some recent evidence points to the fact that vitamin D deficiency might also predispose you to develop early osteoarthritis. But that hasn’t been fully proven as yet.
There are many discussions in the scientific literature about other possible articular cartilage softening in the knee joint. Many of these scientific articles think that there may be a metabolic cause at hand. They think that our ultra-processed food chain leads to the presence of more baseline inflammation in our body and knee joint. This seems like a reasonable explanation for some. It does appear that many of the chronic diseases we are seeing an increase in have a metabolic cause. Issues such as heart disease, dementia, fatty liver, type 2 diabetes, etc all appear to have a metabolic component that can be tied to metabolic issues and our food environment which has us constantly eating highly processed foods.
Muscular weakness is also felt to have a role in the development of articular cartilage softening in the knee joint. Cartilage health can change rapidly in response to exercise. It appears that exercise stimulates the production of our bodies own anti-inflammatory chemicals such as Interleukin-10 (IL-10). IL-10 is felt to have cartilage protective features and is a potent anti-inflammatory. The concentration of IL-10 increases in the knee joints of people after exercise. This may be one of the reasons why exercise improves knee pain in may people.
Treatment Options for Chondromalacia:
The treatment of chondromalacia will vary depending on how severe it is. Not everyone with softening of the patella cartilage has pain. In cases of mild chondromalacia, with minimal cartilage damage, physical therapy and exercises to strengthen the muscles supporting your kneecap can be very effective. As I mentioned above, the benefits of exercise cannot be over-emphasized. Rest is very rarely the answer for people with anterior knee pain.
In addition to stimulating the production of our body’s own anti-inflammatories like IL-10, other tests such as an MRI have shown that rest can actually lead to cartilage thinning. Exercise can lead to an improvement in cartilage health. When I talk about exercise I am referring to both aerobic and resistance exercises. Walking is a great form of aerobic exercise, but it is not a good form of resistance exercise. Resistance exercise involves bodyweight exercises or some forms of weight training. Working with an athletic trainer or physical therapist is important so that you can learn the proper exercises and their proper form.
A compression sleeve often offers relief to many chondromalacia sufferers. If you are a runner and experience pain in the front of your knee, minimizing hill running, changing your running technique (toe vs heel runners) can be effective as well. On occasion, we might inject someone who is very uncomfortable and their knee is swollen and very painful.
If your patellar pain is due to instability, maltracking or a patellar dislocation, this video will help you understand your treatment choices.
Can Chondromalacia be Cured?
At this time the answer is (sadly) no. We do know that our diet and exercise influence the health of our cartilage. Therefore it is important to avoid ultra-processed foods and eat a diet of real food with plenty of fruits and vegetables too. Exercise can help your body to repair itself. It turns on the production of your internal anti-inflammatories, and it helps the cartilage strengthen itself. The pain from chondromalacia can often be treated. Common treatments for chondromalacia include:
- Physical therapy
- Compression sleeves- used to try and decrease pain while you start an exercise program
- injections
- Gel or Hyaluronic Acid
- PRP or Platelet Rich Plasma injections.
- Surgery:
- Arthroscopy ( very rarely necessary)
- cartilage regeneration: microfracture, cartilage replacement (only for those of you with significant cartilage holes or thinning)
- Tibial tubercle osteotomy (big operation, and only for those with a significant cartilage loss under your patella)
Most patients can lead very active lives after treatment is started. You do need to commit to an exercise program for a while. You might not start to see improvement for 2-3 months. There is ongoing very active research into medications that appear to show promise in reversing or halting the progress of chondromalacia or arthritis. Wnt inhibitors are medications that may be available over the next 3-7 years. Early data shows that Wnt inhibitors might eventually be able to reduce or cure arthritis. Very exciting recent development.
Can Chondromalacia be treated?
YES! :-) There are many treatments and remedies to help minimize the pain and knee discomfort associated with chondromalacia. Exercises, dietary modifications, medications, physical therapy, and (rarely) surgery can help minimize your discomfort and let you lead a happier life in minimal discomfort.
Further questions?
Reach out to me via comments, Twitter @hjluks or Facebook