
You woke up one morning, and your shoulder is hurting a lot! You also notice that it feels a little stiff. How could this happen ?!?! You do not recall a significant injury. A frozen shoulder is a stiff and often very painful shoulder.
A frozen shoulder moves less than your normal one. If a physician diagnosed you, they might have mentioned the term adhesive capsulitis. That’s the formal name.
The cause of a frozen shoulder is still a bit of an unknown. There are many theories, and we will dive into that in just a few minutes. While some frozen shoulders might follow an injury, most new cases of painful, stiff, or sticky shoulders have no apparent cause.
Many people avoid moving their shoulders because it hurts; most of you will stop using the shoulder because you are afraid of hurting it more. In a frozen shoulder, that is the opposite of what you should be doing. People who have been diagnosed with a frozen shoulder will not cause harm by moving the shoulder.
We are now going to go over why frozen shoulders occur, and approaches for how to treat them.
Not all stiff shoulders are frozen shoulders. That might be a tough one to grasp. We will get into this later- but some people have neuro-inhibition, pain, inflammation, and so on, which decreases their shoulder motion. The difference is that in a real frozen shoulder, the structures inside the shoulder lock it up so you cannot move it.
In this post, and the videos below, we are going to learn about the most common causes of a frozen shoulder, and how you can overcome it. Many of you can expect to recover fully over the next few months— yes, many months. Unfortunately, some people will not recover rapidly and may need our assistance.
At the bottom of this post will be several videos and stretches to further assist you in stretching your shoulder.
What Is a Frozen Shoulder?
It is not hard to diagnose a frozen shoulder. The criterion needed is simply that the shoulder is locked up, stiff or sticky, and moves less than a healthy shoulder should. X-rays are often normal, so this isn’t part of an arthritic process.
Very early cases of a frozen shoulder might be more of a challenge to diagnose. That’s because the pain often precedes the stiffness. So you may see your doctor complaining of severe pain, but stiffness isn’t present yet. The stiffness tends to follow the pain by a few weeks. By the time many of you get to a sports medicine doctor’s office, the stiffness has started to set it in.
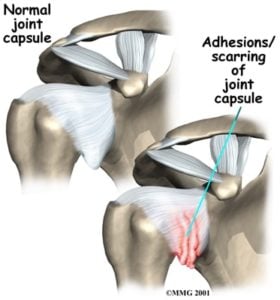
So, we do not entirely understand why a frozen/stiff shoulder occurs. Most people will not recall any event or injury which preceded their stiffness and pain. The stiffness occurs because the capsule or the ligaments that hold the shoulder joint together becomes very inflamed. Then the ligaments surrounding the shoulder joint start to shrink and thicken.
As the ligaments thicken, you lose your ability to move the shoulder comfortably. Because of the inflammation, attempts to move the joint can cause severe pain. If we were to look inside a healthy shoulder with a camera, everything would be white and pristine. If we look inside a frozen shoulder, everything is red, inflamed, and thickened. The capsule or lining of the joint would have a very angry appearance.
An MRI will show inflammation and thickening of the joint capsule. The joint capsule is the ligaments and tissues that hold the shoulder together. See the picture on the right. The MRI will show thickening and inflammation of two regions, the rotator interval, and the axillary pouch. I mention this because many of you get a copy of your MRI reports and like to know what all the words on the report mean.
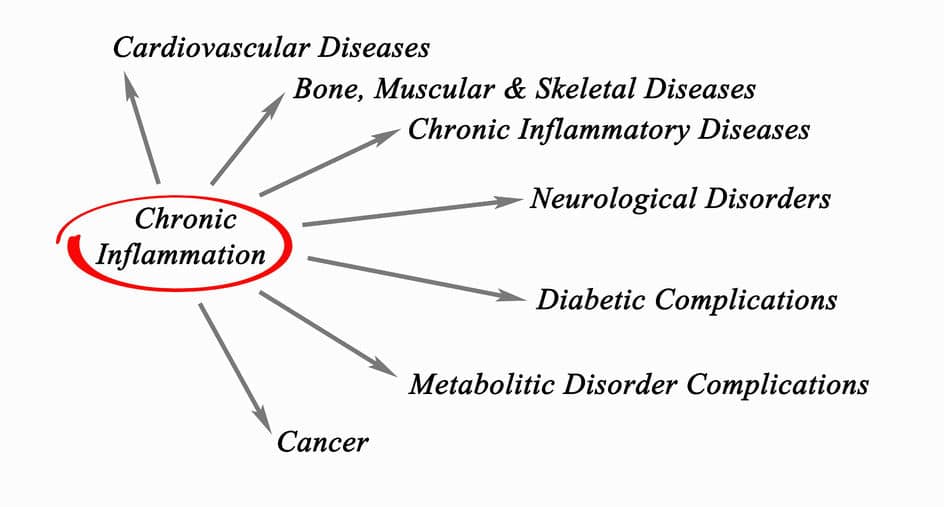
Perhaps 1% of people will develop a frozen shoulder. Most people who develop frozen shoulder are over 40. This is also when we start to see the onset of chronic diseases associated with inflammation. Issues such as type 2 diabetes, metabolic syndrome, heart disease, etc.
Many of the above conditions contribute to a high degree of chronic inflammation in the body. Some of the issues mentioned above are caused by inflammation. All these conditions must be related. We are highly complex beings– and the biology that governs our function is likewise very complex. To look at individual systems, and ignore the concept of the entire person would be a mistake.
Women suffer from a frozen shoulder more than men. The reason why this is the case is not apparent, at least to me.
Diabetes and frozen shoulders
People with diabetes are far more likely to develop a frozen shoulder. Upwards of 25-20% of people with a frozen shoulder will have diabetes. Nearly 12-15% of people with diabetes will develop a frozen shoulder in their lifetime. This helps us in determining what the possible cause of a frozen shoulder is.
People with diabetes have high sugar loads in their bodies. This causes chronic inflammation. Type 2 diabetics often have other medical issues such as metabolic syndrome.
The metabolic syndrome is comprised of abdominal obesity (a big belly), hypertension, glucose regulation issues (hyperinsulinemia), and lipid disorders. Both diabetes and metabolic syndrome significantly raise the degree of chronic inflammation within the body. A frozen shoulder is a highly inflammatory condition… perhaps all of these conditions are related?
Why is the rotator interval, and the shoulder capsule so sensitive to inflammation? Why does diabetes affect shoulder motion more so than any other joint? We are not sure, but other orthopedic issues are similar.
A Dupuytren’s contracture is a disorder that affects the palm. The “connective tissue” in the hand hardens, stiffens, and contracts. That causes bumps in the hand to occur and gradually causes loss of motion in some of the fingers.
Dupuytren’s contracture, diabetes, and frozen shoulders seem to be somewhat related… perhaps all have the same metabolic etiology or cause?
Chronic inflammation causes many other orthopedic issues. It can lead to osteoarthritis, and it can lead to tendon problems too. But the severe inflammation and the acute, sudden onset of pain set a frozen shoulder apart from other orthopedic conditions caused by poor metabolic health.
Injury, surgery, and stiff, painful shoulders.
Another frequent cause of stiff, painful shoulders is injuries to the shoulder. Especially those that require any period of immobilization. Anyone who had a rotator cuff repair and developed severe stiffness that took months to resolve can attest to this.
Fractures, repairs, and surgery are often followed by a period of time in a sling or shoulder immobilizer. The injury and surgery cause bleeding; bleeding can lead to scarring. Surgery involves messing with the capsule or ligaments of the shoulder. That insult to the capsule or ligaments can cause them to become stiff, inflamed, and painful- leading to a frozen shoulder. Injuries, fractures, and surgery also cause acute inflammation (different than chronic inflammation). That acute inflammation can cause the capsule of the shoulder to become thick, painful, and stiff.
Some people come through surgery of recovery without developing stiffness. Go figure. Why some people develop stiffness and others don’t is intriguing. There is undoubtedly a genetic component to it. Some people produce more IL-6 and other inflammatory chemicals in response to injury than others. Some people have chronic diseases that cause chronic inflammation, so it would follow that they are at a higher risk for developing a frozen shoulder after an injury.
Injections and painful, stiff, frozen shoulders
Injections seem to be associated with the onset of a frozen shoulder. There are many theories about why that occurs, but no one truly knows for sure. Frozen shoulders can start from an innocuous injury that you barely recall. Perhaps just the injection itself serves as a trigger to initiate a frozen shoulder.
Infections can cause a stiff, painful shoulder too. Not all infections are characterized by pus, swelling, redness, and warmth. Some infections cause chronic, indolent inflammation but do not create pus, fevers, or other signs we typically associate with infections.
The shoulder seems particularly susceptible to a bacteria we call P. Acnes. This is a troublemaker for shoulder surgeons. This bacteria lives deep in the hair shafts. That makes it impossible to kill them when we clean your skin for surgery. You could bathe in betadine or alcohol, and you still wouldn’t kill all the P.Acnes on your skin.
There are many docs in the shoulder community that think that P. Acnes may be causing some people to have prolonged pain and stiffness after surgery around the shoulder. Can injections cause an infection? Sure. It’s not common, but it’s possible. Could a frozen shoulder following an injection be due to an infection? Maybe. I’m not sure, but I think it’s possible
Neuroinhibition and stiff shoulders
Not all stiff shoulders are frozen shoulders! Some people have a pseudo-frozen shoulder. Say you fall, and your arm is forced up or to the side. That will cause a muscle strain, or perhaps a tear. The pain created by the injury can initiate a process where the nerves from the brain and the spinal cord shut down the electrical signals to the muscle. The lack of electrical impulses will make it hard to move your shoulder.
Imagine a light bulb… it’s a 60W bulb on a 120-volt circuit. Now, cut the voltage in half. The bulb will not be as bright. The brain and spinal cord can do the same thing. They control the nerve signals to your muscles. Those nerve signals are electrical. So if the muscles are not getting a full-strength signal they will not work well.
This nerve inhibition can present like a frozen shoulder, but it is not an actual frozen shoulder. As your pain improves, and as your nerve conduction returns to normal, your range of motion will improve.
What causes a frozen shoulder? Did I do something wrong?
In most situations, you woke up one morning, and your shoulder was bothering you. The initial phases of a frozen shoulder are not usually associated with stiffness. That means that you may still have normal motion in the shoulder. A frozen shoulder is also associated with significant sleep abnormalities. If you are a side sleeper, you notice that you can not get that arm up and under your head. Your sleeping position did not cause your frozen shoulder.
A frozen shoulder is more likely to be due to a lack of activity rather than too much activity. An activity might cause sprains and strains, but it doesn’t cause a frozen shoulder. The vast majority of people do not use the shoulder as part of an exercise regimen. This may play a role in why a frozen shoulder is so common. But, this concept has not been proven- and likely never will be.
If you have metabolic syndrome, type 2 diabetes, Afib, and other diseases known to be due to metabolic issues, then perhaps your diet and lifestyle do have a causative role in your frozen shoulder. But, you do not have a frozen shoulder because you did too much work around the house, or worked out too often.
If my shoulder is frozen, why does my neck hurt too?
The process started when your shoulder started to hurt. Then you noticed that the range of motion of your shoulder was diminished. Now your neck hurts. Are these issues all connected? Did the frozen shoulder cause a neck problem? No, it didn’t.
The frozen shoulder didn’t cause a neck problem, but it can cause muscle aches around the neck. It may not initially seem obvious why that’s the case… so here’s the explanation for that.
If you cannot move your shoulder normally due to stiffness, then your body will try and compensate for that. You will start to move your scapula or shoulder blade more than you usually do. The scapula is elevated by the trapezius muscle and a few other smaller muscles. Those muscles are now working harder than they ever have before. That will inevitably lead to discomfort around the base of your neck or trapezius.
Once your shoulder motion is restored, then you can often expect the pain along your neck and trapezius will go away too.
A Stiff and Painful Shoulder
A frozen shoulder can cause very severe pain with severely limited motion in some people. Other folks might have a more mild variant and not have severe stiffness. A frozen shoulder progresses through 3 phases of development and resolution:
I. The (painful) freezing phase.
During the freezing phase, you will have severe pain, but your motion is not very restricted. What’s happening inside your shoulder is that the lining of the joint, what we call the capsule, is becoming very inflamed. If we could look in with a camera which we see a red, angry appearing capsule. This inflammation causes severe pain because when you try and move the shoulder, you are stretching this inflamed joint capsule.
II. The frozen phase.

A thicker capsule will make it harder to move your shoulder because it is not as flexible or giving as a normal capsule is. Think of a thin rubber band versus a thick and heavier rubber band. It is much harder to stretch the thicker band. During this phase, you will notice that washing your hair, putting on a coat or a shirt, or reaching up to get something out of a cabinet can be difficult.
Do you have questions regarding an Orthopedic injury or longevity?
Do you want to talk to an expert who can listen to you for 45-60 minutes and explain the options in detail?
Dr. Howard Luks offers remote guidance sessions to review your X-ray or MRI images and explain your options.
Dr. Luks has also received hundreds of requests for educational sessions on the topics discussed in his book, Longevity Simplified.
A good way to visualize what is happening in your shoulder is to look at the picture on the right. It shows you shrink-wrapped meat. Imagine that the capsule of thin tissue that surrounds your shoulder suddenly shrinks to half its normal size. That’s what is occurring in a frozen shoulder. Your shoulder joint is being shrink-wrapped.
III. The thawing phase
The thawing phase of a frozen shoulder is when the tight and thick capsule and ligaments in your shoulder begin to loosen up. The capsule is starting to become thin and flexible once again. During this phase, your pain will diminish, and your motion will improve. Below you will see stretches you can review with your doctor to see if they are appropriate for your frozen shoulder.
Stretching and exercise are the most successful way of treating a frozen shoulder. Unfortunately, most patients with a stiff and painful joint will not try and move it out of fear they are causing harm. That’s a normal response to an injury. In a frozen shoulder, it is safe to assume that you run very very little risk of injuring yourself by stretching.
How Do You Treat a Frozen Shoulder?
Once you start treatment for a frozen shoulder, you will often begin to see improvement in your pain within weeks to months. People with diabetes have a much longer time course. Non-diabetic frozen shoulders may fully resolve within 4-6 months. On occasion, it can take up to 12 months or more for your full motion to return. Unfortunately, a frozen shoulder can cause permanent stiffness too. This is more likely to occur in people with diabetes.
We do not know why improvement in your shoulder motion might take much longer in some people. Many of you spent weeks not moving the shoulder or not using it in fear that you were hurting yourself. Now that you understand that pain doesn’t always imply harm, you can get going on your recovery exercises.
For some reason, a frozen shoulder may not fully resolve in diabetics, despite long term treatment, including surgery. Because inflammation is the issue that led to the shoulder capsule becoming stiff and thickened, many of you will notice a significant improvement in your pain and stiffness after a steroid injection is placed into the shoulder joint itself. That is not an easy injection to give because the joint is so small so that an ultrasound-guided injection might be recommended.
The most important part of the recovery process is a carefully structured stretching program. An injection might help diminish the inflammation, which makes the stretching exercises easier to tolerate. Far too many people are afraid of moving their shoulders because they are afraid of causing more harm. Therefore as a physician, the most important thing we can do is educate you about the natural history of a frozen shoulder. This should alleviate the fear of causing harm.
We are there to act as a support and guide as you work your way through this. Recent studies have shown that a carefully guided strengthening program can also improve your frozen shoulder symptoms. This is interesting as we used to avoid strengthening exercises initially during the recovery process. The thought here is that strengthening causes stretching of the capsule while applying weight — theoretically leading to a better stretch.
Surgery For A Frozen Shoulder? Usually not.
Surgery is rarely needed for a frozen shoulder. We consider surgical intervention if injections, stretching, and physiotherapy is not resulting in improvement in your shoulder pain or your shoulder motion. The decision to proceed with the surgery is a quality of life decision.
When we operate on a frozen shoulder, we will manipulate the joint to stretch or rip the tight tissues. We will then place a small camera in the shoulder and use a small device to open the ligaments, which allow them to stretch back to their normal position. Although shoulder surgery for a frozen shoulder is successful for many, it is not always as effective as we would like it to be. Many are left with some residual loss of shoulder motion; this is especially true in diabetics.
Recovery Process For A Frozen Shoulder: Often longer than you think.
Once the inflammation has diminished, physical therapy and stretching become critical to helping you alleviate the stiffness and recover. Many people believe that they should limit their use and motion of the shoulder when it hurts. When you have a frozen shoulder, the opposite is true. Typically, the more you stretch it the, more rapid your recovery should be. After a steroid injection, your shoulder pain is usually less, so that you can stretch your shoulder more effectively.
Most patients will respond very favorably to physical therapy. Be prepared; it also takes a lot of patience since recovery from a frozen shoulder can take a long time.
Occasionally patients fail to respond to therapy and injections. In those patients, manipulation under anesthesia, or surgery (arthroscopy) to release the tight capsule might improve your stiffness. Again, in diabetics, you may not respond to the therapy or surgery. The surgery for a frozen shoulder is called a capsulotomy. This means that we release the capsule of the lining of the shoulder, making it longer and hopefully, more comfortable to move.
Many of you who have the surgery will wake up and notice that the shoulder still feels stiff. That’s because the release doesn’t result in immediate changes. It will still take time for you and your physical therapist to stretch the shoulder capsule further even after the release.
A frozen shoulder is a very frustrating and challenging condition for many people.
If you have a painful, stiff shoulder, there is a good chance that you have a frozen shoulder. Seeing a shoulder specialist to rule out other causes of stiffness and pain might be a good idea before starting an aggressive stretching program.
This video includes some straightforward stretches…. talk to your doctor to be sure about your diagnosis and the appropriate treatment you need first.






















Carla
Dr Luks-
This is Dan’s story: On February 4th, 2017, my twenty-two year old son had a AC shoulder separation while snowboarding. If was his left shoulder, he’s left handed. The on sight doctor examined him, took an x-ray and diagnosed a level 3 separation. At that time he wore a sling, iced it regularly, took pain medication when needed and began physical therapy. After eight weeks he saw a shoulder specialist who felt the injury was leaning towards a level 5 separation. He felt Dan was progressing nicely, had good range of motion. If he saw Dan the day of the accident he would have recommended surgery, yet felt it unnecessary at the present time with the progress Dan made. It’s roughly six months late Dan is back to his active life, kayaking, rock-climbing and doing occasional construction work. All things considered he seems to be doing well. He doesn’t sleep on his left side yet due to discomfort and has occasional pain. I understand Dan isn’t your patient, and you’ve never met, my question is this: Can someone with a level 3 or 5 shoulder separation recovery successfully without surgery. We know cosmetically the bump will always be their. Is there a time frame when a person should consider surgery? Is it an option one, two or three years down the road? Your thoughts would very much be appreciated.
Thank you for your opinion
Gratefully, Carla
Sounds like he’s doing very well. Doesn’t seem like surgery needs to be considered now… surgery will not become harder to perform than it is now if the need arises (due to pain) in the future.