Show Notes
Paul and Howard talk about sports injury imaging, from x-rays and MRI, to ultrasound.
Topics:
- What are the main tools for imaging injuries?
- When are these tools most useful? When are they not?
- Why Paul thinks he should be on a frequent imaging program
- The future of imaging, from machine learning, to handhelds, to potentially doing it less routinely
Readings:
- You cannot unsee your MRI report
- Should We MRI All Patients With Joint Pain?
- Video: How dangerous are magnetic things near an MRI?
Music:
“Crossing the Chasm” by Kevin MacLeod (incompetech.com) licensed under Creative Commons: By Attribution 3.0
Disclaimers apply (at the end of the episode).
About The Show
Simplavida is about smart services and tools for simplifying longevity. Its co-founders are Dr. Paul Kedrosky and Howard Luks M.D.
Paul Kedrosky is a frequently injured athlete and a venture capitalist. Howard Luks is a top sports orthopedic surgeon. Smart, candid, and experienced analysis, ideas and tips about health, fitness, and longevity from two athletes and sports orthopedic surgeon—and guests.
Listen & Follow
Trascript
PAUL: [00:00:00] This was a revelation to me that you might use imaging for splinters.
HOWARD: [00:00:05] You can’t unsee your MRI result
PAUL: [00:00:10] I realized in the last week I’ve been, I’ve been imaged twice, have like some frequent imager. I was x-rays last week cause I broken a toe. And which I didn’t realize by the way, it was like I had gone off and decided it was fine and was running again, and then realized that, what, it’s not fine and it’s pretty seriously not fine. Got it imaged , but the allegation was it was broken. we’ll see what happens. And then of course, today’s episode was getting some stuff removed from a finger.
HOWARD: [00:00:36] You’re good for my profession.
PAUL: [00:00:39] I am very good, although I don’t, I’m not so good for orthopedic surgeons. Historically, they mostly just image me and leave me alone because it turns out they can’t do anything.
HOWARD: [00:00:47] Your day will come.
PAUL: [00:00:49] That’s nice. That’s very reinsuring. what I find interesting about imaging is there’re so many different reasons we do it. I didn’t even realize imaging is used for things like this with splinters, for example, if you can’t locate it immediately, apparently I am told, as I discovered today, that they sometimes use ultrasound to figure out where the heck the thing is because they can’t locate it and they don’t want to go digging around and they’ll, they’ll start doing ultrasound for that. This was a, this was a revelation to me that you, you might use imaging for splinters.
HOWARD: [00:01:16] I love ultrasound. it’s really become an amazing tool of late. We don’t see many splinters or foreign objects on x-ray. so the ultrasound becomes our go to, strategy.
PAUL: [00:01:30]Yyeah. who knew it’d be so useful. I guess what’s interesting to me beyond the splinter problem is the reasons why people get imaging. I imaged, I find super interesting, and I’ll speak for myself first, is that obviously there’s this acute problem. There’s the splinter, there’s the, the knee tweak, there’s the whatever. There’s also the other side, which is, it can be a feminist, is not to be cynical, but it can be a fairly useful procedure from the stand of doctors. Because if I don’t have a good answer and you won’t go away, a good way to punch you out of the office is to send you off and get some imaging done. Right.
HOWARD: [00:02:01] Well, that might be a good way to get you out of the office, or it might be a good way to guarantee that you’re going to come back often
PAUL: [00:02:10] That’s true. you’ll come, you’ll come bouncing back. The, the other one that I find interesting is the idea that, and I see this a lot, I’ll hear this from people, and you see this a lot in pro sports, there’s this knee jerk tweak, no pun intended, that that an athlete has an injury on it or something goes wrong on a Sunday. And fans are all huddled around or some sub Reddit trying to find out what they, if they done the scan yet, have they done the scan yet? Is there anything we learned anything about what’s happened to this brain and it’s this almost, I don’t even know, palliative reassurance that people get from knowing that the scan was done, not even really cares. What it says is just that you had the scan, right?
HOWARD: [00:02:45] Professional sports is a whole, whole different arena, right? You have to image them. You’re paying a lot of money for them. You want to know what’s going on. Are they playing next week or not? But it sets the bar really high when regular people come to the office and we don’t offer them the opportunity to have an MRI, as soon as they come in for an evaluation.
PAUL: [00:03:05] So let’s go through the top types of imaging you see most often in orthopedics. I mean, I’ll, speaking for myself, I think I’ve probably been x-rayed more often than I’ve been MRI. I’ve been ultrasound a couple of times, CTS never. That’s so I would say if I had to make a loose Billboard style, top three or four list, it’s x-ray, MRI, ultrasound, and then nada.
HOWARD: [00:03:31] X-ray is definitely first. we are in the habit of X straying. Most joints, even first-time evaluation, certainly after injuries. we’ve come, come back and forth, with the auto score for ankle sprains, should we actually or shouldn’t we actually. Most of us will x-ray any, any acute injury. and certainly, if a pain persists. So if you have spontaneous pain in the knee, you wake up one day and you come in and we try some Advil for a few days. That doesn’t go away. If you bounce back to the office, you’re getting an extra I love ultrasound. I think that’s starting to hit a crescendo in popularity, because it’s really a point of care device. You can now have a good portable unit for as little as $2,000 that I can plug into my phone and my iPad and immediately image you and tell you if your hamstring is a vault. And I can do that on the sideline of a soccer game.
PAUL: [00:04:40] Let’s jump to the two big and expensive machines. MRIs and CT scans are really impressive to people. I often think just because it feels like there must be something important going on here, given all the noise they create. if someone tells you they started off with a, if someone thinks that they’ve got a knee injury or something, does it surprise you that they get sent for an MRI?
HOWARD: [00:04:58] It’s infuriating that they get sent for an MRI first, especially. Take you and I, right? We come off a trail, we wake up the next morning and our knee hurts. And for some reason we go to see our orthopedist, or our primary care doctor and an MRI is ordered. So, forget the fact that we haven’t waited and seen if just the tincture of time is going to work, but, they haven’t even gotten an extra day. Because I don’t want to be that orthopedist who ordered an MRI on a severely arthritic knee.
PAUL: [00:05:37] And you’ve got no history, right? You have no idea what was there before. At least at least, if not, if there, maybe if there are longterm patients you’ve seen for other things, but otherwise, no idea.
HOWARD: [00:05:47] Right. we accept the fact that we need glasses, our hairline recedes and we wrinkle and we age on the outside, and somehow we can’t accept that anything is wrong on the inside. And we have a plethora of age-appropriate findings in joints, and sometimes it’s quite challenging to determine if these are acute fresh, or has it been there for 10 years? Is it the cause of pain or is it not to cause a pain? So an MRI can create as much trouble as it can, solve problems.
PAUL: [00:06:22] Are there ever, do you ever, is there any use for CT for you outside of particularly traumatic high-energy things?
HOWARD: [00:06:29] Oh, yes. So, take for example, shoulder instability. So, shoulder dislocations, you’ve had four, five, six. and what we’re learning now is the failure rate is often associated with bony changes on the glenoid or the socket. and so we will CT some of these shoulders to see what the alignment is, and what, and how that will guide our procedure. are, we, we do use CTs.
PAUL: [00:07:02] You can’t get that from MRI or x-ray.
HOWARD: [00:07:04] You can, but it’s not nearly as beneficial. You’re not going to see the same clarity in terms of the focus of how well the bone appears.
PAUL: [00:07:17] So let’s dive deeper into MRI, because that seems to be the one that leads to the most mischief — most helpful and most mischievous in some ways. I don’t know. What do you think it’s particularly good for? I mean, I look at it and I think that the fact it can get inside soft tissue, you can get inside joints. All of these things, all else equal are useful if you already have a bias to think that there’s something there that you need to know about, right.
HOWARD: [00:07:44] Yes. Ultimately, the perfect use case for an MRI in my practice, sports medicine practice, is to confirm my suspicions. So in a classic case, I’m talking to an athlete. I’m going to know the diagnosis. before I’m done talking to them, my exam should confirm it. Let’s say it’s an ACL tear. We know that there are certain common injuries that can occur. At the same time, I may not be able to tell based on my exam if they exist. So if we’re going to be planning an operation, then an MRI is critical to help you plan that operation appropriately.
PAUL: [00:08:28] Right, but you’ve already got a bias to say are based on the following, the following tests that I’ve done during a physical exam, there seems to be some laxity, some looseness in the join. Did the nature of the injuries. Just that there’s possibly an acute injury, you’ve got a pretty good idea before the MRI even happens.
HOWARD: [00:08:46] Yes. If you don’t have a good suspicion of what’s going on, you’re probably not gonna learn much from the MRI. Yes, they can be useful. but they’re also going to show things. So one thing that drives me nuts are adults, 56th year olds, with labral tears in the shoulder. So the labor room is a cartilage disc, and by the time you reach our age, most people have a torn labrum. It’s not the cause of your pain.
PAUL: [00:09:17] I’m proud of my torn labrum. I’ve been thinking of getting t-shirts about it.
HOWARD: [00:09:19] I’ve had one since I was 20. Yeah. I’m still throwing balls and Frisbees and everything else and doing my push-ups and pull ups, but you can’t unsee your MRI result. So that 60-year-old tennis player gets an MRI, sees on the report that there’s a labral tear, what do you think he or she is going to think? Every time they serve the ball and their shoulder hurts, they’re blaming that labral tear.
PAUL: [00:09:46] Yeah. So, well, let’s, let’s come back to that in a second. There’s an amazing YouTube video, I think it’s fromGermany, where the experimenters were throwing various things inside an MRI machine. So, which sounds ridiculous, but it was actually interesting. It’s got a few million views, I think, and he started off with a stapler, and the headline is MRI machine hates stapler. They throw it inside, and it goes ping, ping, ping, ping, ping around inside, and it completely destroys the stapler. And then they step it up a notch. They have like a desk chair. and it actually got up to 2000 pounds of pressure pulling the chair into the MRI machine before the chair basically exploded. As an MRI veteran, if you go in the checklist of stuff that they ask you about now in terms of the kinds of implants and the devices and whatever else you might have in your body right up to things like having a piece of metal in your eyes. Is it possible? You were working on these questions would be like, “Oh my goodness, it is possible I have a small piece of metal in my eye and I don’t know.” And you start panicking. These are pretty amazing devices, but don’t come without their own issues, like metal objects moving around. There are also issues with obese patients as well.
HOWARD: [00:11:10] Oh, yes. And these things, as you said, do not come without, without risk. And unfortunate. All these lists of do’s and don’ts come from bad experiences. Very bad experiences.
PAUL: [00:11:25] Yeah, there was one, I saw another case not too long ago, I forgot why. I’m a buff for this. I guess there was a CHP officer years ago who had, had not told that he had a hidden firearm. And so whenever he got in and he had put the firearm down and put it on at one of those tables that are often inside the MRI chambers, and they turned on the magnet. Well, of course the gun just went, what, ting across the room into the machine. Fired twice. No one was hurt, but the machine was destroyed. It’s just note to self: No hidden weapons.
So let, so let’s jump over to the unseen problem because I think this is, is so important, and I’ll give my own example, which was years ago, I, I think I had had an MRI on my right knee and it was, it was quite sore from an ultra run I had done. It was purely speculative. It hadn’t gotten better after a while and so I had imagining done. And on the report, it said, I had “joint effusion”. And so, I was like that’s it. I knew it. I knew I had joint effusion. I knew it all along. This was the problem. And then I thought, “What the hell is joint effusion?” Right? It was not exactly common parlance, and you realize this is just a little bit of fluid or some swelling, which could have been there all the time. It might’ve just happened because of this long event, but it’s probably gonna go away. But it was really, really tough to unsee the image, but also to even un-see the radiologist read of the image.
HOWARD: [00:12:54] Yeah, I have my own experience. It’s the same thing. I did a long run, I tweaked my right knee, I hyperextended it. My knee was swollen. I had an infusion. And it hurt for two, three months. Finally, I stepped into a magnet. There’s a meniscus tear as well as a cartilage injury. Like, that’s it. My running is done and all of a sudden, three weeks later, swelling, gone, pain gone. I’m back on the trails and running. But in the back of my mind, even with all that I know about the fact that most meniscus tears don’t need treatment, I’m always thinking whatever I twist that knee, that the meniscus tear. I can only imagine what it’s like for people who don’t understand the natural history of these issues.
PAUL: [00:13:39] So, I’ll play devil’s advocate because there’s this spirit of open data, we’ll loosely call it, and people want to see their data, their images. You never used to be able to, and now they want to see it. They want to bring it. They want to look at the report. It’s all available. Some would say, all right, I’ve heard people say this. The tried to keep people from seeing these things is just the medical business circling its wagons and being paternalistic and saying, You’re too stupid.
HOWARD: [00:14:04] I think it’s going the other way, actually. They’re actually trying to get radiologists to sit with patients to review it. I think that creates a whole host of problems for the patient, the surgeon and the radiologist.
The radiologist might know that there’s a meniscus tear. They may not know that we don’t operate on the majority of tears on 50-year-olds. Same with rotator cuff tears, same with labral tears. So they can certainly sit there with the patient and delineate what they see on the MRI. But I don’t imagine that most have the training to put it all in context.
PAUL: [00:14:49] So in, in, in Howard’s perfect world, how would you handle that?
HOWARD: [00:14:54] Yeah. I really implore my patients before I send them to the MRI, I tell them very specifically, this is what I am looking for. Your MRI is going to say this. And it would have said this a year ago before you were injured last week. So I’m not going to care about these little things that are going to show up and that I anticipate simply based on your age. I’m looking for X, Y, and Z, and I’ll spell it out. Then I implore them, please do not grab your report, hit Google and panic. Just come into the office. We’ll go over your images. I’ll explain what I see.
PAUL: [00:15:39] Yeah. And that’s, that’s such an important point, that last bit about the copy and paste from the radiologist report into Google. The way I always phrase it to people, and I was just saying this to a running friend the other day, is that there’s a survivorship bias there. If you think about who posted the thing that you’re now finding when you search online, and there are some very active knee and hip forums online, for example, where a lot of patients, people who’ve found something wrong or think they found something wrong or been operated on. Those, these are not the people in general who are out running, doing other things, and feel like everything’s fixed. Why? Because those latter people are too busy doing all those other things. And so the larger population of Google search results for any constellation of symptoms has hugely overrepresented in it people who have problems that involve the keywords that you’re searching for. By definition. The pool’s polluted with that kind of data and there’s no way around it. And yet people don’t realize that when they start searching for these things.
HOWARD: [00:16:44] Yes, I have a very active websit; it gets a ton of traffic and I’ve tried to rank for keywords, in these areas, and it’s really hard. You either get these Q&A sites where it is the unhappy people or the people that are not doing well, and for whatever reason they’ve chosen to share their experiences. And then you get the people who are buying these keywords: you need an operation, we’re happy to do it, etc. So it’s really hard to get meaningful, actionable, useful information to bubble up on Google.
PAUL: [00:17:30] That’s such an important point that people don’t understand, how that stuff gets there that you’re searching for. It doesn’t even require cynicism by the people putting it there; it’s just an artifact of the overrepresentation of injured people among the people who are discussing things. I mean, I had retina surgery years ago. and everything went fine. Knock on wood, but I don’t post about it. But if you go out there and search for the exact procedures that I had done, I guarantee you it’s a nonstop horror story. People who’ve had all kinds of complications, loss of vision, and so on. Horrible. This is the nature of the medical search beast, whether it’s orthopedics or ophthalmology.
HOWARD: [00:18:17] Absolutely. We face the same issue with physician rating sites. You have a great, experience in a doctor’s office. You’re off and moving on to your next thing. You’re not going to jump on Google and praise them.
PAUL: [00:18:34] Let’s talk a little about innovation and changes in imaging. We talked a little bit about how ultrasound is becoming cheaper and more portable, and that’s probably a good thing. MRI, on the other hand, I don’t know if it’s becoming cheaper. My sense is it’s not much cheaper and it’s definitely not more portable magnets or great big, awful things, but the magnetic field involved is ratcheting up. We had two, one and a half to two tesla fields, and I don’t even know what we’re up to now, maybe five tesla. My concern with this stuff is the subtleties of what you’re finding are just so minute that the opportunity to find things that have absolutely no practical meaning are legion at these field strengths.
HOWARD: [00:19:19] Yeah. it’s a race to the bottom. How many little things can we find and describe. You’re going to find lots of things. People go for second opinions on their surgeon’s recommendations. They don’t go for second opinions on their MRI readings. I’m not even sure they can, but they should, because depending on the imaging center, you might have your scan read by someone who reads breasts, belly, brains and shoulders. You’re gonna get a different read from them.
PAUL: [00:20:03] And you’ve got time of day effects. There are all sorts of wonderful papers showing that radiologist reads or are influenced by day, day of week and time of day, and these are material impacts.
HOWARD: [00:20:14] Very much so. And in my world, I very much rely on pertinent negatives. So if you say the MRI says small degenerative meniscus tear, but doesn’t mention 10 other structures in the knee. I’m just going to assume you didn’t look at it. I’m, I’m not going to assume that you looked at it and it’s normal cause there are some subtle things that do bother people that I really want to know. If you looked at, know, not all knee pain is meniscus too, so I need to know more about the knee than just the status of the meniscus. So, as a mature sports surgeon, I certainly have my favorite radiologists and imaging facilities.
PAUL: [00:21:01] I had an, an orthopedic guy once tell me, and he said it quite proudly, which I was amused, because It was completely dismissive: He said, I never look at any radiologist’s report, ever.
Do you have questions regarding an Orthopedic injury or longevity?
Do you want to talk to an expert who can listen to you for 45-60 minutes and explain the options in detail?
Dr. Howard Luks offers remote guidance sessions to review your X-ray or MRI images and explain your options.
Dr. Luks has also received hundreds of requests for educational sessions on the topics discussed in his book, Longevity Simplified.
HOWARD: [00:21:11] Ah, so I look at every radiologist report. Because I’m not perfect either, and those reports have saved me and save my patients. On a shoulder x-ray where there’s a mass in the, in the chest. something totally unexpected. and so I absolutely look at every image myself. I look at every x-ray, every MRI, but I’m also going to look at the report.
PAUL: [00:21:40] Right. Why not? They see a lot of images, by definition. It struck me as a lot of chutzpah, super macho. These men and women see a ton of these sorts of images, and then sometimes it helps to have a large, as they say in the machine learning world, a large corpus of data to pull from and dismissing it seems a bit ridiculous. But it didn’t surprise me either.
Let’s step back from imaging a little bit to thinking about the next generation of sports surgeons coming along. For example, does this reliance on imaging make it harder to train people? What are are you seeing in terms of people’s instinct to race straight to images, and if it isn’t on the image, it isn’t there or vice versa. I don’t want to rely on the physical exam until I’ve seen an image.
HOWARD: [00:22:28] Yeah. we’re very much, in the middle of a high tech, low touch medical environment. one that I, rail against on my website and saddens me. Because it’s not unusual to hear patients complain that they tried to schedule a visit to see another surgeon and they insisted on an MRI first. And as for residents, the residency review committees, and a lot of the directors, they focus on the number of cases, the breadth of cases, the type of cases, the variation of cases, enough complications, etc. Not necessarily on why that, that patient that they’re operating on is in the operating room. So if you’re a resident and you’re fixing five rotator cuff tears with me on Friday, so you might therefore assume that everyone who comes to my office with a rotator cuff tear is ending up in the operating room. So it becomes quite a challenge.
PAUL: [00:23:31] How do you talk young doctors off the ledge of thinking that, before they can say anything even remotely definitive, that they need that, that image?
HOWARD: [00:23:47] My own experience has morphed dramatically, from much of the same reasons. We were in clinic, often unsupervised, as trainees. and yeah, I was 20 something years old. I really didn’t know that much, and I’ve, my training has come full circle from being high tech and low touch to being high touch and low tech and occasional tech, tech when necessary.
PAUL: [00:24:21] Do you think your cohort is the last of a generation who has a appropriately skeptical view of imaging? Or are the cows out of the barn? Is this all just fighting a rear guard action here? There’s nothing we can do about it.
HOWARD: [00:24:34] That’s a great question. There are a bunch of young orthopods who are on Twitter, who I’ve come to know over the last year, and I’m very happy to say that they’re railing against this imaging of every knee or shoulder that comes into their clinic. They are tired of having to resort to getting an x-ray only after an MRI has been obtained. They clearly get that we could have made all the clinical decisions that are necessary to treat this person based on the x-ray. And then you have a lot of older folks, a famous sports surgeon whose most famous line is, If you want an excuse to operate on an athlete, all you need to do is get an MRI. So the word is certainly getting out there. But in a productivity-based health care environment, which is fee for service and will stay that way for a long time to come, the more service, the more fees. There is certainly appropriate need for imaging and I certainly obtain enough MRIs to keep our imaging center busy, but it’s certainly not the majority of people come in my office.
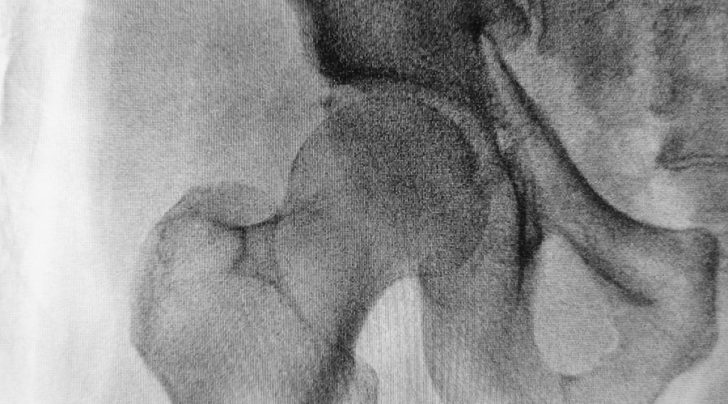
PAUL: [00:25:57] Yeah. I was, for a while, fairly optimistic about this stuff. I used to feel like cheaper MRIs were a good thing and higher magnetic fields. We’re going to give us better images. And I now feel less so, as I see more and more of the research in this area. I was reading something not too long ago about the incidence of femeroacetabular impingement among young athletes, I think it was Danish soccer players under the age of 20, seeing if they had it, one of the two varieties.
HOWARD: [00:26:27] Cam and pincer.
PAUL: [00:26:29] The incidence was, was like low teens or something like this and it was completely asymptomatic, so it was irrelevant. And yet I don’t think people have really got it into their heads yet, the wild diversity of structures in the body that look like they have some kind of pathology are actually generally asymptomatic. And asymptomatic even sucks as a wor. I was saying this to someone the other day that when you describe some unusual body structure that seems slightly outside the norm as asymptomatic people’s immediate reaction is, Well, that means one day it’ll become symptomatic, right?
HOWARD: [00:27:06] There’s no doubt.
PAUL: [00:27:08] Yeah. It’s just the whole word makes them think, Oh, I’m going to go from a symptomatic to symptomatic because you use that word. And what’s striking though is that it isn’t just aging athletes like you and I, it’s young people too that have these structural quirks. And the more, the more intensive the imaging, the more of these we discover and the more opportunities for trouble.
HOWARD: [00:27:29] Sure. Yeah. And parents, right? Everyone is the parent of a superstar athlete. “You don’t understand doctor. They are the best on the team.” Right? I mean, have you ever walked into an orthopedics office and insisted on an MRI? I get that all the time
PAUL: [00:27:50] Yeah. And if you don’t, it’ll show up in a Yelp rating. I’ve seen this in Yelp ratings. I went in, there was a problem. I couldn’t get them to do an MRI. I had to go to a different doctor.
HOWARD: [00:28:01] So yes, it will show up in a Yelp rating, but worse, it shows up in scores. And those are scores that if you’re a hospital employee, that’s going to come back to bite
PAUL: [00:28:16] Just, yeah, hard to see how this gets sorted out, because I think about this in the context of instrumentation of people and everyone walking around with sleep & HR monitors and tracking all sorts of bio indicators. And I think we’re going to go through this feeling like everything’s broken and needs to be fixed. Maybe they will eventually grow up and realize being broken is part of our charm.
HOWARD: [00:28:38] Right? I think this is a good role for insurance. Yes, they do block imaging far too much, however, if I think that a large number of imaging studies ordered because of the discussion as to why it’s not necessary, it’s going to take 10 X longer. Someone might be inclined to order that test, but the insurer is going to say, What’s your indication? Right? You haven’t tried X, Y, and Z. It’s only been hurting for three or four days, so come back in a month,
PAUL: [00:29:16] So there it’s a complexity problem that maybe ensures by being so high bound and slow moving in some way, solve the problem for themselves by being unwilling, unwilling to do anything.
HOWARD: [00:29:26] It could be, but they’ll go, they go too far.
PAUL: [00:29:29] But maybe having someone there playing blocker on this stuff isn’t such a bad thing. Cause I, as we go towards build of portable ultrasound, five tesla MRI, ubiquitous, ubiquitous imaging … this is a very different place from even persistent monitors of heart rates and other things. Because we’re looking deep inside and there’s an awful lot of structures in there that are pretty unusual from person to person.
HOWARD: [00:29:54] Without a doubt we are an over-diagnosed, over-imaged society. and that unfortunately leads oftentimes to over-treatment, which undoubtedly is going to lead to major complications. But the thoughts of being a medical conservative and how to approach being so is starting to be reborn again. So there is some hope.
PAUL: [00:30:20] Well on that modestly hopeful note, let’s leave it there.
HOWARD: [00:30:24] Okay, Paul.












