As many would agree, we are an over-tested society. Who is driving this? Are docs ordering more tests because it is easier than explaing the natural history of many injuries? Do patients insist on techno-imaging studies “just to see what’s going on”? Yes :-) Most instances of over-testing in Orthopedics, I venture to say are not due to fear of mal-practice. It is not the standard of care to image every ache or pain… nor does every ache or pain usually require anything more than a thorough history and physical exam. Many studies show that a well performed interview and exam is usually more often correct at arriving at the diagnosis— or at least equally successful — than an MRI or CT.
So the next time you go to the doctor’s office… think twice about asking for an MRI, and ask why an MRI is being ordered.
As usual… this is not meant as medical advice… nor does it represent the opinion of my employers…
As requested…. transcript.
Good morning. I hope many of you on the eastern sea board, enjoying a warm day home. And for those of you like me brave going outside, hope you made it to office safely.
Over-testing
While rounding in the hospital this morning, someone who I work with quickly pulled me aside and showed me an MRI. And on that MRI was a cartilage tear or meniscus tear in the knee. And then the question was asked …”my brother who lives in India needs surgery”. They mention that their brother was told by a number of surgeons that surgery was necessary and that it should be done sooner rather than later, yeah, yeah, yeah.
I asked a simple question, does your brother have any pain? Answer, no. He plays badminton five to seven days a week and he does have pain — it does not have any affect whatsoever on his quality of life. Now, does that patient needs surgery? No.
Why did that patient have an MRI in the first place? He went to his physician complaining of knee pain after a vigorous day in the gym on the day prior and an MRI was ordered. Now a tear was identified and now surgery was being recommended for pain that ended up subsiding on its own after two days of relative rest.
Over-utilization
So, this brings up a very big topic; a topic that I’m very interested in and a topic that is all the rage in social media. It focuses on our propensity towards over-treatment, certainly towards over-utilization. Associated with that are significant risks. And what if the specialist who sees that MRI doesn’t necessarily delve into the effect that the meniscus tears are having on the patient or their quality of life. Does the patient needs surgery because something (non life threatening) was identified on the MRI?
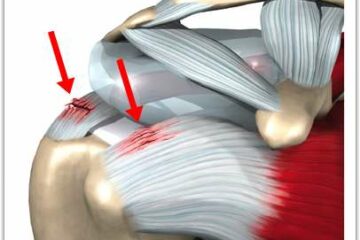
Certainly, if it’s a tumor, etcetera, you need to do something, certainly if it’s an aortic aneurysm or you have something bleeding into your head. Okay…. BUT, I’m an orthopedist and what I’m talking about are predominantly orthopedic issues. Furthermore, I’m talking about issues associated with the fact that as we get older — our parts wear out. Most rotated calf tears are attritional, the tissue simply wore out. Most meniscus tears are degenerative. The tissue has simply worn out. Most attritional rotator cuff tears and degenerative meniscal tears or cartilage tears in general do not bother people, or if they do, they certainly do not bother them enough to warrant surgery, which can have its own consequences.
Associated costs
Now, imagine if surgery is indicated and a pre-operative work up is done, some blood study might show an abnormality and which might trigger other tests. You see, where I’m going with this. Not every person who walks into our office needs an MRI. Why is an MRI is ordered then? It’s a lot faster to sit there, push on someone’s joint and then say to order an MRI then it is to say let’s wait for two weeks and see if your symptoms are going to go away on their own. And, you know what, they usually do. It’s a lot easier to order the MRI than it is to sit there and explain why an MRI is not necessary.
And certainly there are reasons to obtain MRIs— persisting pains, certain weakness patterns, instability of the knee, the knee is buckling and giving away and thus it leaves you at risk for falling. And certainly I’m not offering medical advice, I’m simply saying just because you have a few days of knee or shoulder pain, don’t look for an MRI. And if one is ordered, and you have a co pay of 200, 300, 400 dollars whatever it is, consider not having it done, consider waiting and seeing if the pain subsides spontaneously. Certainly if there is something else such as a tumor that your surgeon is thinking about, I would go ahead with the study, of course!!!
But for simple aches and pains and injuries that are triggered by our activities of daily living, there is nothing wrong with waiting, and then find a physician who is going to treat you…. Then make some other decisions. There is a different personality to every injury. Not all injuries behave the same way in every one. You can have someone with an anterior cruciate ligament tear without instability, you can have someone with rotator calf tears without pain and without weakness and without any night discomfort. Not all meniscus tears require a surgery, not all rotator calf tears require surgery. I think by now you got to gist of where I’m going. So I’m going to stop. I hope you have a wonderful day. I’m going to go home and get my kids outside and probably lose a big snowball fight all three of them. Bye.













OK…I’ll bite on your Twitter comment.I agree with you basic premise that a “well performed interview and exam is usually more often correct at arriving at the diagnosis— or at least equally successful — than an MRI or CT. “The problem is that the evidence clearly suggests that a “well performed” medical interview is more the exception than the rule at least among primary care physicians. I have seen plenty of studies which have looked at physician fulfillment of patient requests (driven by DTC advertising and the like) and the results show that while some physicians acquiesce to such requests, most physicians are able to deflect those requests which are clearly unreasonable. While I don’t condone over testing, I can certainly understand why patients would ask for an MRI or CT if they are worried enough to see a physician. Fear of cancer. Every one of us knows of at least one person who died of cancer that was somehow missed by their doctor (personal physician). Tests like MRIs and CT scans are the tools used to diagnose cancer so why not get scanned. After all… as the scenario goes, my neighbor had a pain every time she did XYZ and her doctor told her to stop doing what caused the pain…and she was dead of cancer in 2 months. Kent Bottles post in Healthcare Business Blog spoke eloquently to this kind of problem. If and when physicians regain the moral high ground by communicating better with patients, helping them understand their choice and providing them with the support they need and want to self manage their chronic conditions, I expect patient trust will increase and imaging request will decline. In the mean time, everyone person I know is quickly coming to realization that they can’t depend upon their doctor to do what’s right or in what their best interest anymore. It’s an unfortunate situation.
I agree with you… and my own personal observations are that physicians are guilty more often than patients, when it comes to requesting advanced imaging studies.