Physical therapy is the most critical aspect of your overall recovery from an ACL rupture.
Why do I need physical therapy after my ACL reconstruction?
You would be surprised at how often that question arises. Many people do not understand that how we jump, pivot, land and train has a lot to do with our risk of developing an ACL tear in the first place. If you have torn your ACL you are at risk for re-tearing your new ACL or tearing the ACL in the other knee.
The surgery to reconstruct your ACL is important … that is why the surgeon you choose matters. That is also why these 4 tips are critical when you have suffered an ACL injury. BUT, that is only a small part on your long path back to the ballfield. Your physical therapist has the most important job in guiding you after your ACL reconstruction. Physical Therapy is clearly the most critical part of the overall ACL recovery process …
Let’s see what our experts have to say.
Why is Physical Therapy Important After an ACL Reconstruction?
Trent Nessler : @ACL_Prevention : Website ,blog
Physical therapy is critical for the patient to achieve their optimal outcome. Most patients (>95%) do not know what to do following an ACLR and therefore need the guidance of a skilled physical therapist to aid them in achieving optimal outcomes. Working with the right skilled therapist will help the patient achieve their maximum potential and significantly reduce their risk of re-injury when they return to sport. That said, there are several phases of rehabilitation, all which have well published goals/objectives. Included here are a few additions for the first five stages for the athletic ACL population.
- Phase I-II (0-4 weeks)
- Goals are several fold including inflammation reduction, gain TKE (terminal knee extension) and restore normal gait pattern (way we walk).
- All the goals are important but as little as 5 degree extension lag will alter gait. So there is a lot of focus on restoration of TKE and normalizing gait pattern (stride length, TKE at heel strike and cadence).
- Due to the impact on lower extremity kinematics, core training is started right away as well as some form of cardiovascular training
- Low level proprioceptive retraining and SL activities are started as indicated per protocol or when cleared by physician. This aids in building limb awareness which many times is lacking well before the injury itself.
- Phase III (4-6 weeks)
- Goals include control swelling, maintain TKE, increase knee flexion and progressive strengthening.
- All goals are important but a significant portion of athletes continue with a lateral shift with bilateral squats and decreased confidence in the involved limb 12-14 weeks post op or even when they return to sport. This is a major risk factor so starting to train early aids in reducing. So neuromuscular retraining is started at this point. This includes correction of lateral shift in squatting motion (body weight only and only in range can be performed without pain) and closed kinetic chain single limb activities.
- Neuromuscular retraining is KEY with all exercises. Ensuring proper kinematics with lowest level of exercises to higher level. Prevention of adduction in the frontal plane is constantly emphasized with any exercise.
- Use pain and swelling as a guide.
- Phase IV (6-10 weeks)
- Goals include control swelling, maintain TKE, increase knee flexion and progressive strengthening/proprioception.
- All goals are important but including hip proprioception and closed kinetic chain strengthening for the gluteus medius is key. Manual proprioceptive retraining for the core and while in single limb CKC exercises is key to progression to the next step.
- Phase V (10-12 weeks)
- Goals include control swelling, progressive strengthening/proprioception and prep for running in next phase.
- All goals are important but ground reaction forces transmitted through the limb with running = ~2.6x body weight. Therefore maintaining stability in single limb performance and preventing adduction in the frontal plane is key. Progressed from low level of plyometric activity to higher. More aggressive manual techniques include more manual proprioceptive retraining including full body work and single limb work.
Sylvia Czuppon : @czuppons : Website :
I think it’s first important to emphasize that physical therapists are movement experts. We are trained to break down and examine every aspect of the movement system. It is my belief that without physical therapy post-ACL reconstruction, patients will ultimately develop compensatory movement patterns that will put them at risk for subsequent injury either to the same knee, opposite knee, or another lower extremity joint. Without PT, it is unlikely a patient will return to their pre-injury level of activity – which is often the reason the patient elected to have surgery in the first place.
Typically, the task of even walking correctly is a challenge that is not mastered for weeks after surgery. In the first stage of rehabilitation (typically 0-6 weeks post-op), it is critical to reduce edema, gain full knee range of motion and normalize functional activities such as getting up/down from a chair, walking and climbing stairs. In the second stage of rehab, I stress strengthening the trunk and lower extremity, balance, flexibility and cardiovascular conditioning. The length of time patients spend in this stage varies greatly depending on motivation, compliance and ultimate goals but is usually anywhere between 6-24 weeks post-surgery. The third stage of rehab involves exposing patients to jumping, cutting, and running. Although not every patient having surgery is a competitive athlete, every patient should pass this stage as these are common activities people perform even recreationally. The final stage, reserved for athletes, includes exposure and practice of sport-specific movements and tasks. Activities in this stage are highly variable but focus on technique, power and performance. Proper technique and movement quality is essential throughout every stage of rehabilitation, which needs constant monitoring by a trained professional such as a PT.
Julie Eibensteiner : @laurusrehab : Website
The surgical fix is a physical one. The physical therapy component certainly helps with regaining range of motion, decreasing pain/swelling, and building physical strength but the retraining of the brain and how it interacts with the body is often what most people fail to appreciate. Most ACL injuries are non-contact in nature, people aren’t getting injured because they have a “weak” ACL, they are getting injured because their body is failing to control forces on it which are ultimately too much for the knee to handle. In essence, it is how we are interacting with the ground and our environment; especially when decelerating (stopping/cutting/pivoting/
Anja Goebel : @ACL_not_again
In order to assure a successful outcome of your ACL reconstruction a guided rehabilitation is of utmost importance. PTs/ATs will steer you safely through the journey of your recovery, sometimes pushing you beyond what you think is possible while other times holding you back from doing things that might jeopardize your graft. We are your cheerleaders and your biggest fan and provide a shoulder to cry on if you need it.
I divide my rehabilitation protocol into 5 main phases. I am not giving timelines for the phases because everybody advances at a different pace.
During the first phase of your post-op rehabilitation the goals should be to control pain and swelling, improve ROM and regain full extension, to reactivate the quad muscles and posterior chain. This is also the time and to reestablish a normal walking pattern that progresses from assisted to full unassisted weight bearing. During this phase I introduce patella mobilizations to prevent adhesions and once the patient exhibits good quad control I start simple single leg balance on solid surface. This promotes proprioception as much as it reestablishes the patient’s trust in using the involved leg. The ultimate goal is to be able to perform a perfect straight leg raise, which initiates a gradual progression into phase 2.
During the second phase of rehabilitation the main focus lies on regaining basic strength, proprioception and normalizing the gait. This includes lots of hip and core strength, more focus on posterior chain as well as a progression from concentric to eccentric strengthening. Proprioception makes up a good amount of exercises during this phase, evolving from stationary stance on solid ground to movement patterns on differing surfaces. I am a stickler about perfect form and rather have a patient perform fewer repetitions perfectly than a lot of reps with poor form. I continue with patella mobs and do some soft tissue mobilization on portals and incision once those are completely healed.
While continuing core strength exercises throughout the entire rehab process, phase three is introducing some functional and agility training while continuing to increase strength in the reconstructed leg. The focus now is definitely on eccentric control and the transition from single plane to multi-plane exercises. This is usually where rehab begins to be fun for athletes, because, skipping, bounding and simple ladder drills awaken the athlete inside of them and boost their confidence in their reconstructed knee. They usually return to reality with the ever-evolving proprioceptive balance exercises that will challenge postural control and endurance. When you see a patient in phase four of an ACL rehab, you will ask yourself what they are doing in PT, because they are functioning so well. This second to last phase prepares and reconditions the athlete to return to their sport. Progression from double leg to single leg jumping and landing, starting and stopping, as well as cutting and pivoting in a controlled environment are the main emphasis of this phase. Of course basic strengthening and balancing exercises continue to play a big role as well.
Once the athlete exhibits good control in all of the categories of phase 4 I gradually return them to their playing surface. I discuss the practice plan with their coaches and allow them to participate in certain non-contact drills until they transition into full practices after being cleared by their surgeon and pass the return to sports test.
Darin Padua: @DarinPadua : Website
Rehabilitation following ACL reconstruction consists of various stages / phases that should be goal oriented. The Sports Medicine Research Laboratory at UNC Chapel Hill worked in collaboration with our Sports Medicine staff to develop a phased approach to the rehabilitation process, based on the best available evidence. We are continually studying this process.
Phase 1 (0-6 weeks):
- Control and minimize swelling and pain
- Goal: pain less than 2 out of 10
- Restore knee motion – focus on extension
- Symmetrical active range of motion
- Restore quadriceps function / activation
- Able to complete 3 sets of 20 reps of straight leg raise with no extension lag
- Address weight bearing status
- Single leg balance on firm surface for 1 minute (no errors on Balance Error Scoring System – BESS)
- Double leg squat to 45-60 degrees, no compensations
- Symmetrical gait patterns
- Restore and maintain patella complex mobility (patella, patella tendon, anterior interval, fat pad, portals)
- Important factor in being able to achieve normal knee motion and restore quadriceps function / activation
- Ensure full ankle dorsiflexion range of motion
- Ankle dorsiflexion with knee extended = 20 deg
- Ensure full hip mobility – focus on extension, rotation, and abduction
- Hip internal rotation = 45 deg
- Hip external rotation = 45 deg
- Hip extension = 5 deg below horizontal
- Hip abduction 45 deg
Phase 2 (6-14 weeks):
- Maintain symmetrical and optimal knee (especially extension), hip and ankle mobility
- Maintain control over swelling (none) and pain (less than 2 out of 10)
- Improve balance
- Single leg balance on foam surface for 1 minutes (minimal errors on BESS)
- Restore quadriceps strength
- 80% of uninjured side
- Single leg squat to 30-deg without compensations
- Develop lumbo-pelvic-hip complex stability
- Symmetric strength for hamstrings and gluteals
Phase 3 (14-20 weeks):
- Maintain symmetrical and optimal knee (extension), hip and ankle mobility
- Restore quadriceps strength
- 100% of uninjured side
- Single leg squat to 60-deg without compensations
- Develop eccentric control and ability to safely decelerate
- Single leg hop to stabilization (tri-planar) without compensations
- Double leg jump landing (LESS score < 2)
- Develop overall lumbo-pelvic-hip complex strength
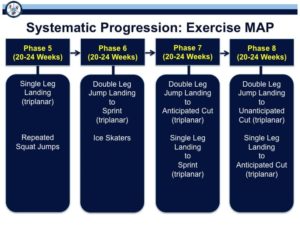
Phase 4 and beyond the focus is to maintain mobility and strength (no regression) and focus on achieving excellent movement quality across a spectrum of activities. During these remaining phases a Movement Assessment Progression for Exercise – “Exercise MAP” – can be used. An overview is provided in the figures below.
Do you have questions regarding an Orthopedic injury or longevity?
Do you want to talk to an expert who can listen to you for 45-60 minutes and explain the options in detail?
Dr. Howard Luks offers remote guidance sessions to review your X-ray or MRI images and explain your options.
Dr. Luks has also received hundreds of requests for educational sessions on the topics discussed in his book, Longevity Simplified.
Jesse Dimick : @Jdimick : Website
Post op Physical Therapy is important to ensure optimal outcomes. PT will help guide you through each stage of your ACLR. Instruction in appropriate exercises for each stage is key to protecting the graft, increasing ROM, decreasing edema, increasing strength and decreasing risk of future injury.
Phase 1 (0-2 Weeks post op)
- Protection of the reconstruction
- Attain full knee extension
- Decrease knee swelling
- Promote quad strength
- Gain knee flexion ROM to 90-100 degree
- Weightbearing as tolerated per MD
Phase 2 (2-6 weeks post op)
- Begin strength work (Quad, post chain, hip, core)
- Knee flexion of 120 degrees or more
- Normalize gait pattern without crutches
- Closed chain exercises
- Increase muscle endurance Bike/elliptical/
treadmill walking
Phase 3 (6-12 weeks post op)
- Maintain full ROM
- Walk with normal gait
- Single leg strength work
- Some athletes are cleared to run at 12 weeks
- Make sure athlete is normalizing weight distribution with strength work
- Regain full muscle strength
- Increase overall conditioning
- Sport specific training
- Progress single leg strength
- Initiate plyometric and jump training
My thoughts: You suffered through the injury to your ACL. You suffered through the pain of the surgery itself. Hopefully this (long) post clarifies just how critical the role is for your physical therapist in the overall recovery process. The last thing in the world you want to do is to have to repeat this process again. How well you and your therapist work together will have a lot to do with your recovery, confidence and ability to get back in the game with as little risk of re-injury as possible.













Cathryn
Hi my name is Cathryn I am 16 years old and I tore my meniscus is my left knee last May and had surgery on it. Then I went back to playing basketball in July and on the second day of the tourney I tore my acl in the right leg. I had surgery the last week in July and have had to sit out of volleyball but now that basketball is coming back I really want to play. So in two weeks I will be getting my brace so I can start playing but Im worried I will mess it up. Lately I have been running and working out but my knee has been making some really weird popping noises and it feels loose. I don’t know what to do because if I ask my doctor or physical therapist he might not let me play in two weeks and I really dont want to lose my spot on varsity.Please reply and give me an honest opinion. Thanks.
Cathryn,
Even in best of circumstances you would not be allowed to return to basketball yet. 4 months simply isn’t enough time. There’s no way your knee or your psychological well being (doubt, fear,etc) is ready. There are well described tests to determine when people can attempt to return to sports. No one would pass them at 4 months. Returning to sports now means that you would stand a very high risk of tearing your new ACL. Plus, if the knee feels loose now I would get another opinion to be sure the ACL is working well.
I’m very sorry to be the bearer of bad news, but it takes at the very minimum 6-9 months before the best rehabilitated athletes can return to play after ACL surgery. A brace will NOT protect you.
HJL
Cathryn
Thank you it means a lot.
Brandon N
First thank you for writing this it is very helpfull for me, Im 17 and a senior in high school and want to heal my injury as best as possible. I completely tore my ACL and just had surgery 2 weeks ago I was put in an immobilizer for a week while icing my knee and using a passive motion machine I just got a new brace the one i think i will use for the rest of my recovery (dont know the term/name for it). But my problems is the physical therapy my parents insurance was switched with there new jobs and doesnt really pay for much and after the xrays MRI and sugery money is a little tight and I dont know if we will be able to pay for pt what can I do?
Perhaps you can talk with your school’s athletic trainer. You also have the option of meeting once with the physical therapist who can show you what to do on your own. That works for many who have issues with the cost of PT.
Good Luck
Kendra
Thank you for writing such a thorough description of what to expect post surgery, and truly how long it may take. I am female, age 34 and my knee is terribly worn… Meniscus, MCL partial and ACL full tear as an athlete at 13, surgery at 24 when other meniscus tore and now have sustained a second, 2 part repair after ACL became essentially non-functioning at an unknown or un-remembered point in time (cartilage transplant was needed first and was successful). I am hoping this time the PT is more agressive, as it was minimal for surgery in 2006 performed in rural ND. I think this is the second comment alluding to a possible disparity in knowledge and methods due to location….thoughts?
Yanni
I am 15 going 16 and i tore my acl and meniscus. Is it possible for me to figure skate 5 months after the surgery? Will i be able to execute movements such as jumping up and landing on one leg with the landing knee bent?
probably not … but that will be up to your surgeon and therapists to decide
Luis Garcia
Hello, I am 20 years old, and Im schedule to have surgery in june, I would like to know your point of view and which graft to use; donated or my own?
Did you see this post? https://www.howardluksmd.com/orthopedic-social-media/acl-surgery-graft-choice-5-professional-opinion-series/
Deborah
My 14 year old daughter tore her ACL playing soccer on 10/11/15. Her growth plates were still open so we were referred to Lurie Children’s Hospital in Chicago. She had surgery on 11/13/15. The surgeon did a transphyseal ACL reconstruction using a hamstring graft. Prior to the surgery she did a lot of prehab and was in very good shape going into surgery. She had full range of motion and no swelling. She started PT seven days post op, going three times a week for 8 weeks, and at 9 weeks went down to two times a week. Her PT is saying that she is not really benefiting from PT anymore and will stop going at 20 weeks post op. We are scheduled to see the surgeon at that point. I should mention that on the days she does not have PT she does her home PT program, and she was released to run on the treadmill. Her surgeon told her to run every other day, increasing in 2 minute increments each time. She is up to 30 minutes with no pain. My question is what does she do next? I understand that the healing process takes time. We aren’t trying to rush her return to play. The last thing we want is for her to re-injure her leg or tear the other ACL. She feels so good that it is becoming difficult to keep her from doing things that she hasn’t been cleared to do. I have not been able to find a PT who does sports specific therapy in the rural area we live in. There are athletic training/sports enhancement type places, but they are run by an athletic trainer versus a PT. I’ve read about certain testing criteria that are used to assess progress, but neither the PT or the surgeon have utilized any of these tests so far. My daughter loves soccer and basketball. We want to position her for the safest and best return to competitive sports. I feel that I cannot get specific information from either the surgeon or the PT pertaining to what she can and can’t be doing at this point. Or what and when the next step is for her. At 12 weeks the surgeon said she was a full month ahead of what he would expect. Any insight you can provide would be appreciated.
It’s really up to your surgeon. Neuromuscular training, landing, jumping mechanics, etc are critical to avoid re-injuring the same knee or tearing the ACL in the other knee. Your surgeon will put her through a bunch of tests to see if she’s ready to progress.
Good Luck
Naomi
My son had acl repair early October 2015. He’s just been given the all clear to start running. Is it realistic for him to be able to return to rugby next season. He is 20 and plays a high level of rugby. His rehab so far has been on track. Is there anything specific he should be doing or be aware of for the future?
I really can’t comment on when your son can return to sports. There are many criteria and tests he needs to pass before he can be released to sports. The MOON protocol and the MOON group in general discuss this at length in their articles.
Christian
On average, how many weeks post op do people get cleared to run?
varies by graft choice, meniscal injuries, etc. Some at 4 weeks, some not until 8 weeks or more. No rush to get back to running. All the recent research actually shows we should hold off on running longer due to persistent inflammation months after surgery.
Kayla
I am currently a junior in highschool and play volleyball and basketball. I tore my acl mid December during a basketball game an got it repaired December 22. I was wondering what exercises I can be doing to insure a speedy and strong recovery. I would like to be completely prepared for volleyba season in the fall. Is it possible to be playing a sport again four months post op?
Four months is pushing it. You should Google the MOON protocol for an ACL reconstruction and have a PT or Trainer guide you.