
Running is a fantastic sport. Running has been associated with longevity; it improves cardiovascular fitness and enables us to clear the cobwebs from our head after a long day. But running has its downsides too. Most runners will suffer from an overuse injury during their running careers. Overuse tendon injuries or tendinopathies are the most common form of overuse injuries that a runner will sustain.
Runners are a big part of my practice as a Sports Medicine Doc. As an active trail runner, I understand the runners’ mentality. Many of us need to run to feel whole. Yet, runners can also be a challenge to treat. Most runners throughout their life will develop an overuse tendon injury. Tendinopathy is the term used to describe the most common form of overuse tendon injury. Achilles tendon pain, for example, has sidelined many accomplished and amateur runners alike. When I see these injuries in the office, many common themes typically emerge. This article will explore the most common causes of tendon pain in runners. In addition, we will explore other general health and metabolic conditions which elevate your risk for developing tendon pain or tendinopathy. Some of the metabolic issues that can affect our tendons might surprise you.
Many runners execute similar training errors which led to the injury in the first place. Also, many of you will significantly underestimate the time needed to recover fully from an overuse injury. Furthermore, many runners have been told to rest by healthcare folks who don’t specialize in treating runners. Rest may be the worst thing to do for tendon related overuse injuries in a runner, or it may prevent an injury from becoming worse. Hopefully, this post will help clarify how to determine which approach is in your best interest. This post will deal with how these overuse injuries arise, who should stop running, and techniques to work through these injuries.
Tendon response to loading in runners
Running puts a significant amount of stress on our tendons. Pace, volume, and terrain can all increase tendon load. If given enough time for adaptation our tendons will often be able to accommodate an increase in our training volume, our running pace, and changes to the terrain we are running on.

Tendons are a metabolically and physically active tissue. Tendons function to transmit energy to the muscle it is attached to. Tendons are non-rigid, so they can both store and return energy. Tendons will usually respond favorably to a mechanical loading environment such as running. Tendons will become larger in cross-section due to collagen synthesis, and a change in the actual tendon fibers themselves. These adaptive changes take place over time. During a period of mechanical loading, it can take 8-12 weeks or more for adaptations to occur. Excessive mechanical loading– a rapid increase in running volume, pace, etc. is considered to be a risk factor for the development of tendinopathy in a runner.
Why do tendon injuries occur in runners?

Many runners get into trouble because the overall load that they apply to their tendons is increased too rapidly– that’s usually when overuse injuries arise. Load needs to be viewed as a cumulative “area under the curve” issue. That means you need to look at the amount you load your tendon over time— e.g. your run today, your runs this week and over the last month. If your loads increase too rapidly an overuse tendon injury is more likely to occur. Given the amount of time it takes an average runner to recover from a bout of tendinopathy, avoidance is your best treatment.
Common tendon issues in runners
An overuse tendon injury is broadly classified as tendinopathy. The term tendinopathy is not particular to one tendon per se. The most common areas we see tendinopathy or tendon related pain in runners include the:
- Achilles tendon (AT)
- Patella tendon (Jumpers Knee)
- Proximal (upper) hamstring (PHT)
- Gluteal muscles- typically gluteus medius.
Amateur runners and even some seasoned runners typically run too often, and too fast. It’s a combination of the frequency and pace that gets most beginner runners in trouble. Perhaps more important is that most runners do not go through a period of base training or base building.
Base training builds aerobic conditioning (cardiovascular status) and lets your muscles, bones, and tendons adapt to your training slowly over time. Without a base period for heart rate (aerobic) development, and running without a plan to add load slowly throughout the season puts you at a higher risk for developing an overuse injury.

Base training… or Zone 2 running is critical for any runner planning on training to run a distance beyond a 5k. That often involves a 6-12 month period of running at a conversational pace which correlates to a heart rate roughly under 130-135 depending on your age. Over that base period, you will become faster at the same heart rate (more efficient), and your heart, your metabolic processes, and your tendons, bones, and muscles will become far stronger. Your tendons will adapt to an appropriate increase in the load and become capable of handling the greater distance. After base training, you can start to add in speed work and other running drills to improve your pace, and ability to run faster if that is your goal. Forgoing a long period of base training puts you at higher risk for developing overuse tendon injuries and tendinopathy.
Associated conditions and risk factors for tendinopathy in runners
While most tendinopathies can be traced to a training error, there are many other important causes of tendon pain. Some of these issues might make a runner more at risk for developing tendinopathy, even though they are training properly. There are many variables that can come into play that influence your risk for developing tendon related pain in a runner.
- Age: Our tendons change as we age. They respond to stress or load slower. In addition, our tendons start to lose strength, and the muscle may become sarcopenic.
- Metabolism: YES. Our metabolic “health” has an impact on our tendons. Tendinopathy has been associated with lipid (cholesterol) abnormalities, and tendon pain may be more common in people with hyperinsulinemia or type 2 diabetes. The reasons are complex. But just like the walls of our arteries have cholesterol deposited inside them which can lead to a blockage, the same can occur in our tendon. Deposition of cholesterol in our tendon can cause weakness in the tendon structure. Cholesterol can also be oxidized (OxPL) due to inflammation. The combination of cholesterol deposition + inflammation leads to blockages in our arteries, and harmful deposits which can weaken our tendons.
- Cholesterol/LDL and Triglycerides: Elevated lipid levels have been associated with the risk of tendon ruptures, and tendinopathy. Many researchers are currently looking at tendinopathy as a risk factor for heart disease, metabolic syndrome and hyperinsulinemia. All appear to have the same metabolic changes, and some degree of cholesterol deposits in the tendon and blood vessel walls.
- Smoking: Smoking affects every tissue in our body, and our tendons are not spared that damage.
- Diabetes: Either Type 1 or 2. Diabetes and glucose regulation issues affect our tendon architecture. Advanced glycation products (AGE) can crosslink with collagen. When AGEs crosslink with collagen the strength and stiffness of the tendon are compromised. In addition, AGEs will induce a low-grade chronic inflammation which increases the presence of reactive oxygen species and other inflammatory biomarkers. This can further compromise the tendon structure, and interfere with healing within the tendon. We discussed metabolic health and its effects on our muscles and joints here.
- Obesity: Obesity imparts more strain on our tendons. When present with other metabolic issues, the overweight are at increased risk for tendon related pain when exercising or running. In addition, visceral fat, or fat around your midsection is a major endocrine signaling organ. This fat is highly active from a metabolic perspective. That also leads to chronic low-grade inflammation.
- Gout: When you suffer from gout, the pain is caused by crystals forming in your joints or tendons. Those sodium urate crystals usually accumulate in our joints and can cause an intense inflammatory response. Gout crystals can also deposit in our tendons. That will weaken the tendon, and the inflammation associated with gout will bring specific white blood cells to the region which have enzymes and proteins capable of dissolving the collagen. This also increases the risk of tendon pain, and occasionally, tendon rupture.
Medications associated with tendon pain in runners.
Certain medications are associated with an increased risk of tendon or muscle pain. They include:
- Fluoroquinolones: These medications can be very problematic. The risk of developing fluoroquinolone related tendon pain is often higher in people over 50. In some cases, these medications are associated with a higher risk of achilles tendon rupture. These medications, which include ciprofloxacin and levofloxacin, are felt to increase the production of a protein that degrades the integrity of the tendon.
- Corticosteroids: These are commonly referred to as cortisone. Tendons do not like cortisone. Cortisone will decrease the synthesis of collagen and therefore weaken your tendon. Injections into weight-bearing tendons such as the achilles or patella tendon can lead to a rupture or tear of these tendons.
- Statins: Statins have been associated with complaints of muscle pain. But there is emerging research that reveals that statins may influence tendon healing. Atorvastatin administered after the surgical repair of a ruptured (mouse) tendon appears to affect revascularization, collagenization, inflammatory cell infiltration, collagen synthesis, and collagen growth. This is not proven to be causative at this stage. What that means is that people with elevated cholesterol/LDL/Trigs are more likely to have tendinopathy. They are also more likely to be on a statin. So we do not know if your tendon pain is associated with the underlying medical condition or the treatment (statin).
The 4 stages of tendinopathy: Onset through the healing
Once you have developed an overuse tendon injury or tendinopathy, your tendon will go through a predictable process towards resolution. It’s important to understand this process because it will help explain why it takes so long to recover from some common overuse tendon injuries.
The first phase is the injury or the inflammatory phase. During that phase, the tendon may be swollen, warm, and very tender to touch. This is usually the most painful part of the overall biological process of tendinopathy. Managing pain in runners with tendinopathy can be challenging in this phase. Many of you will need to curtail running to let the tendon calm down. That doesn’t mean we eliminate all loads. We simply change the loads according to how well your tendon can handle it. That means we may try isometric exercises to challenge the tendon, but minimize movement of the tendon. If other forms of load are tolerated, then your Physical Therapist will advance you as tolerated. The goal of treatment during the inflammatory phase is to calm the tendon down and minimize the risk of generating further inflammation or damage. This process, if managed appropriately, will last a few days to a week.
The second phase is the reparative phase. Many different cells are being recruited to the area of injury. New blood vessels will grow to bring more nutrients to the region. Dead or diseased tissue will be taken away by our white blood cells too. This phase will last up to a month or so. Your tendon will be regrowing new collagen. Initially, that collagen will be disorganized. That means the fibers will not be adequately aligned, and thus, the tendon is still at risk for further injury. Your PT will be increasing your load during this phase. Properly handling the type of load, the rate of loading, and the speed of loading will help the tendon to reorganize the new collagen and hopefully not set you back during the process. Setbacks are not unusual in this phase. Every runner will not respond to the load or exercise in the same way. This process involves a lot of trial and error. This phase can last a month or two.
The third phase is the remodeling phase or reorganizing phase. This phase can be viewed in two parts. The first part involves consolidating the healing that has occurred. During this consolidation phase, the load you are applying continues to help your tendon realign the newly made collagen to help rebuild the tendon. Load is important. Without load or resistance, your tendon will not organize the tendon fibers correctly. That leaves your tendon at risk for continued discomfort and recurring injury.
The final phase of the healing process is the remodeling or maturation phase. Now the new collagen is in the proper alignment, the tendon architecture is normal. The tendon collagen fibers are not yet at their correct size, nor can they handle what you might consider your normal loading pattern, e.g. a 2,000 vertical feet fast trail run. This is the longest phase, and this can take many months to retrain, strengthen, and condition your tendon. It can take 9-12 months for this entire 4 stage process to mature and run its course. Have faith and stick to the program. If your pain is not improved within 7-9 months, then your physical therapist might suggest speaking with a surgeon, or question if the initial diagnosis was accurate.
What do you do when you have pain when running?
Should I stop running? Should I see a physical therapist or a doctor? These questions should be running through your mind if you develop pain during or after a run. Many overuse syndromes can be nipped in the bud if treated early. It is not a sign of weakness to decrease your training schedule. Forget about that race in 3 weeks. The first thing to consider is which pains can be self-managed and which require prompt attention?
Pain in any of these areas means that you need to stop running and be seen by a doctor.
- Groin pain. Stress fractures of the hip (femoral neck) can be a devastating injury if not recognized early.
- Pain along your lower thigh… usually 6-12 inches above your knee. Although rare, stress fractures of your femur occur in this area.
- Pain along the front of your tibia or shin. This can be close to the knee, a few inches above the ankle or more frequently right in the middle of the tibia or shin. Stress fractures of the tibia are common, and if they establish themselves will sideline you for a long time.
- Pain on the top of your toes or foot. Stress fractures of the navicular bone, or metatarsals, if caught early will heal uneventfully.
Pain in these areas might indicate that you are at risk for developing tendinopathy.
Do you have questions regarding an Orthopedic injury or longevity?
Do you want to talk to an expert who can listen to you for 45-60 minutes and explain the options in detail?
Dr. Howard Luks offers remote guidance sessions to review your X-ray or MRI images and explain your options.
Dr. Luks has also received hundreds of requests for educational sessions on the topics discussed in his book, Longevity Simplified.
- Pain in your achilles tendon… if you have an olive-sized bump you already have achilles tendinopathy and you should start your physio.
- Pain in your patella tendon, located just below your kneecap or patella.
- Pain in the buttock, often where your hamstring tendons attach to the pelvis.
- Pain along the outer portion or lateral side of the knee. Although ITB syndrome may not be classic tendinopathy, you do not want it to become worse by ramping up your training.
- Pain along the medial or inner part of your lower tibia. Although this is not considered classic tendinopathy, medial tibial stress syndrome can also lead to a long recovery if it is allowed to worsen.
If you are developing pain in these regions you should not be advancing your training. You should not be performing intense drills or hill repeats. You should consider seeing a Physical Therapist who specializes in managing runners and determine the best activities and exercises to perform to minimize the risk of harm. In general, continuing to put in some easy miles is ok if you are in this latter group who may be suffering from tendinopathy.
Avoiding stress-related tendon injuries in runners
Tendon pain can take up to 8-12 months to improve in runners. That’s an eternity to a runner. Many of you already know this from personal experience. It is challenging to manage people with tendinopathy. Frustration is common, for both of us! Your best “treatment” for tendinopathy is avoidance. How do we improve your chances of avoiding a prolonged recovery due to a training injury?
Advanced runners know their bodies very well. They know their heart rate despite not wearing a watch or monitor. They know if they are pushing it or not. An advanced runner knows if they are in zone 2, or if they are running at their lactic acid threshold or VO2 max. Most advanced runners avoid putting themselves at risk for developing tendinopathy because they understand the concept of base training and they know how to monitor and track their loading. That being said, even advanced runners might not listen to their bodies as well as they should. If training levels are advanced too rapidly, even advanced runners are at high risk for developing tendinopathy.
Elite runners are at risk. They are at risk because they are training on the razor’s edge. Their coach is pushing them to their limit. They are trying to get the most out of their training while trying to avoid an overuse injury. Often they get it right, sometimes they don’t.
The majority of runners who suffer from tendinopathy are a beginner and intermediate runners. As stated previously, you often run too fast, too often. It is critical to understand that most of your runs should be performed in zone 2. That is a low heart rate. If you do not know your maximum heart rate or do not wear a monitor or watch it is still easy to tell if you are in the right zone. We also refer to this as running at a conversational pace. That means that you should be able to talk with your running buddy without having to catch your breath. For beginner runners, that might be starting off with a walk-run combination. As soon as your heart rates rise too high, you start walking until it recovers, then start jogging slowly again. In a matter of weeks, you are running the entire time as your cardiovascular system adapts.
There are tools available to help you monitor your running loads and determine if you are at higher risk of injury. These tools include:
- Heart rate monitors: if you run with a heart rate monitor for your first few months you will be able to predict your heart rate based on how you feel. These are good for beginners who are just starting out.
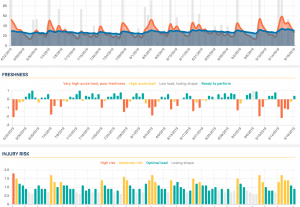
- HRV: I have been using this platform for years and I find that the data and suggestions correlate well with my effort, load, and perceived effort. Many things can affect your HRV or heart rate variability. That includes changes in your diet, your sleep pattern and whether or not you are ill or have certain chronic medical conditions. Certain medications will affect your HRV readings as well. A single number that your HRV app displays aren’t nearly as important as the trends that develop over time.
- Strava fitness: Strava and other apps as TrainAsOne are also able to see how your trends are changing over time. You will be able to tell if your strain (load) is routinely too high in comparison to your “fitness” level- which reflects your conditioning. TrainAsOne can offer you guidance on what type of runs you should do and how often you should do them.














Shannon
Hi Dr. Luks, this is a nice article and really helps me understand the various phases of my recovery from insertional posterior tibial tendonitis/tendinopathy! I’m just about to enter the phase of progressive loading for single leg calf work (after having done a month of double leg calf work, then month of single leg calf work). I’ve caused myself a week long flare up, tender/swollen/irritated, this is just from walking – I’m not even running. I’m doing isometrics to hopefully calm things. Are these setbacks you mention essentially reigniting the inflammation stage? Or more just an irritation, not truly in the inflammatory stage? Does this reset or extend the timeline of things?
Not really Shannon… these “setbacks” are not uncommon. Keep up with isometrics and a heating pad to get it to calm down. Find a distance where walking is tolerated without causing pain and stay under that distance if possible. For some people that may start at two-10 minutes… and then we slowly increase the time walking as long as it doesn’t stir it up. These can be long drawn out recoveries… and I speak from personal experience too.
Kate
Hi Dr Luks,
Thanks for this article. Given we all have different resting heart rates, fitness levels, etc, how does one best determine the target heart rate ranges for each training zone?
Many thanks!
HI Kate.. great question! Using programs like TrainAsOne, they will help find your zones for you. As you follow their program they learn what your response is to run at a varying pace. TrainAsOne will then start to instruct you on what pace to do your long runs, VO2 max runs, threshold and so on runs at.
Alternatively… if you know your maximum heart rate you can also figure out the zones. McMillan and other sites have formulas to assist you as long as you know your maximum heart rate.
Lastly, (but more prone to error) If you have been using Strava for a while, you can look and see what your average heart rate is on long runs.. that tends to be in high zone 2 or low zone 3 for most runners.
Kevin Kellar
I appreciate your article. As a fellow trail runner, do you have any recommendations for a local GP that also understands runners/athletes like yourself. I live the White Plains area. Thank you
Hi Kevin..
I do not :-(. Sorry.