Exercise or physical therapy has been the primary treatment for tendon related pain. Tendinopathy in the most common cause of tendon pain. Has physical therapy worked for your pain? Perhaps it did, perhaps it didn’t. It turns out that standard exercise regimens do not result in improvement in everyone. Many people have persistent tendon pain, and many of you are at risk for recurrence– where your pain returns a few months or years later. Tendinopathy has frustrated many of you and many of the healthcare providers that treat you for decades. But, because of some great researchers, we may be closer to having a new treatment approach that offers a more rapid improvement in your pain, and a decrease in the risk of developing recurrent symptoms. In this post, we are going to explore the basics of the tendon neuroplastic training (TNT) approach to managing people with tendinopathy.
Over the last 5 or so years, research has revealed that the neurological connection between the brain and the muscle or tendon involved may have a significant role in determining whether or not routine rehabilitation exercises will improve the pain associated with tendinopathy. Your nerves are intact and functioning, but it appears that the part of the brain that controls a painful tendon is not sending the proper signals to the muscle/tendon to make it work properly. Let’s explore the new field of tendon neuroplastic training for tendon related pain and tendinopathy.
How are tendons controlled by the brain?
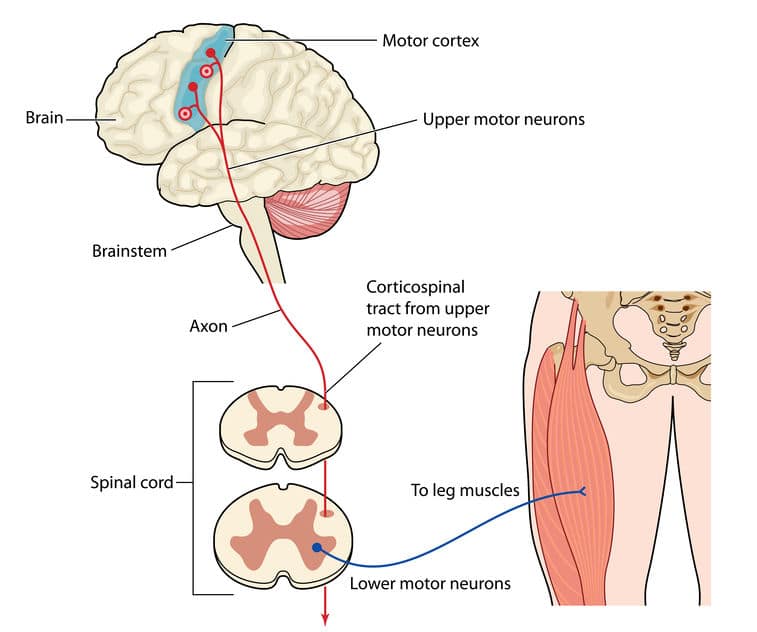
Nerves coming from the spinal cord are called spinal motor neurons, or lower motor neurons. These nerves start in the spinal cord, exit the spine and go to the muscle. In the muscle, there are motor units. These motor units are where the spinal motor nerves terminate or connect to your muscle.
The brain sends out nerves called upper motor neurons to control the spinal motor nerves. In this process, the brain is exerting corticospinal control over the lower motor neurons.
Your brain has nerve cells that control the spinal motor neurons. The brain can have excitatory or inhibitory control over the spinal motor neurons. That means that the brain can stimulate the spinal motor nerves to send a signal to the muscle, or the brain can shut down the spinal nerves.
What is Tendinopathy?
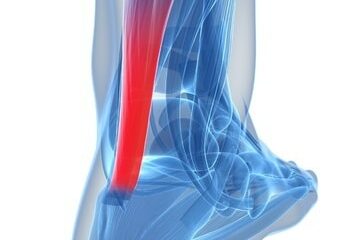
Tendinopathy is a broad term used to describe changes that occur to our tendons and predispose us to have tendon pain. Many of these changes are referred to as being degenerative. Biopsies of tendon tissue don’t typically show signs of acute inflammation. But these biopsies, when looked at under a microscope do show characteristic changes. The changes are typically called tendinosis. Tendinosis refers to “degenerative” or disorganized changes that occur in the tendon as a result of injury, age, metabolic issues, lipid (cholesterol) disorders, gout (uric acid) and people with hyperinsulinemia and diabetes. While we have hundreds of tendons and theoretically all of them can be affected, the most common areas prone to developing tendinosis are:
- The rotator cuff
- The achilles tendon
- The hamstring tendons
- The extensor tendons around the elbow
- the patella tendon
Does the brain have a role persistent tendon pain?

The role of cortical inhibition in recovery from tendon pain or tendinopathy
Weakness is almost universally present in people with pain due to tendinopathy. There have been many studies that have shown that patients with shoulder pain due to rotator cuff tendinopathy have upwards of a 15% decrease in strength compared to their normal shoulder. Runners with achilles tendinopathy and patients with patella tendinopathy also have decreased strength. If those patients did not recover with physical therapy and chose to have surgery to improve their pain— it turns out that their strength deficit persists, even though they feel better. What is happening here? Why are the muscle-tendon units weaker?
As I mentioned earlier, our brain can control the output of the spinal cord to the muscles via the lower motor neurons. The nerves coming from the brain can have excitatory effects on the muscle, or they can have inhibitory effects. That means that the brain may actually be turning off some of the nerve control of the muscle. Muscle strength is often represented by a term referred to as maximal voluntary contraction or MVC. We have always assumed that someone with a decreased MVC or muscle strength is due to pain and lack of willingness to fully contract a muscle attached to a painful tendon. What if the weakness of the muscle is due to a change in the way that the brain is controlling the muscle? It appears that this may be the case. The brain appears to be shutting down the number of active nerves that go to a particular muscle. This process is known as cortical inhibition. Therefore, if only half the normal number of nerve fibers going to a muscle are active, then the muscle is not recruiting all of the muscle cells to contract, and that will limit your MVC or muscle strength.
In many cases of tendinopathy, even if you recover and the pain goes away a strength deficit will persist. Interestingly, you may have a persistent altered motor strategy, meaning that the brain continues to have an inhibitory effect on your muscles. This may explain why people who suffer from tendinopathy experience recurrent symptoms. Fascinating… isn’t it. Let’s move on.
Hyperexcitability and tendon pain:
The opposite of cortical inhibition would he hyperexcitability. That means that the brain is sending too many signals to the muscle via the lower motor neurons. Hyperexcitability has been documented in people with patella tendinopathy or a jumper’s knee and tendinosis of the rotator cuff. But again, we do not yet know whether this hyperexcitability precedes the onset of pain or is somehow related to worsening the issue after the pain occurred.
What is neuroplasticity?
Neuroplasticity is the term used to reflect the fact that our brain changes in response to our lives. Our brain can reorganize itself. It can grow new connections or synapses. Our brain can lose synapses or connections. We can also grow new brain cells (grey matter) in response to a stimulus. Our brain will go through a process of neuroplasticity in response to learning, or injury. This is a very active ongoing process. Our brain’s environment is not as static as once believed.
Tendon neuroplastic training for tendinopathy: Evolution of a concept.
Tendinopathy is a fascinating, and frustrating topic. Chronic tendinopathy is frustrating for countless athletes. It is also very frustrating for the healthcare professionals that treat them. A number of fantastic physical therapists, researchers, and athletic trainers have been researching the area of neuroplasticity and its effects on the prevalence, recurrence and overall treatment of the injured athlete. This was likely brought about by the occasional frustration encountered in managing these patients. It has been challenging to explain why some patients never recover, and why many patients have numerous recurrent bouts of pain brought on by tendinopathy. The science of neuroplasticity and the understanding of how the brain is involved appear to be key in helping craft treatment strategies to address these common tendon disorders.
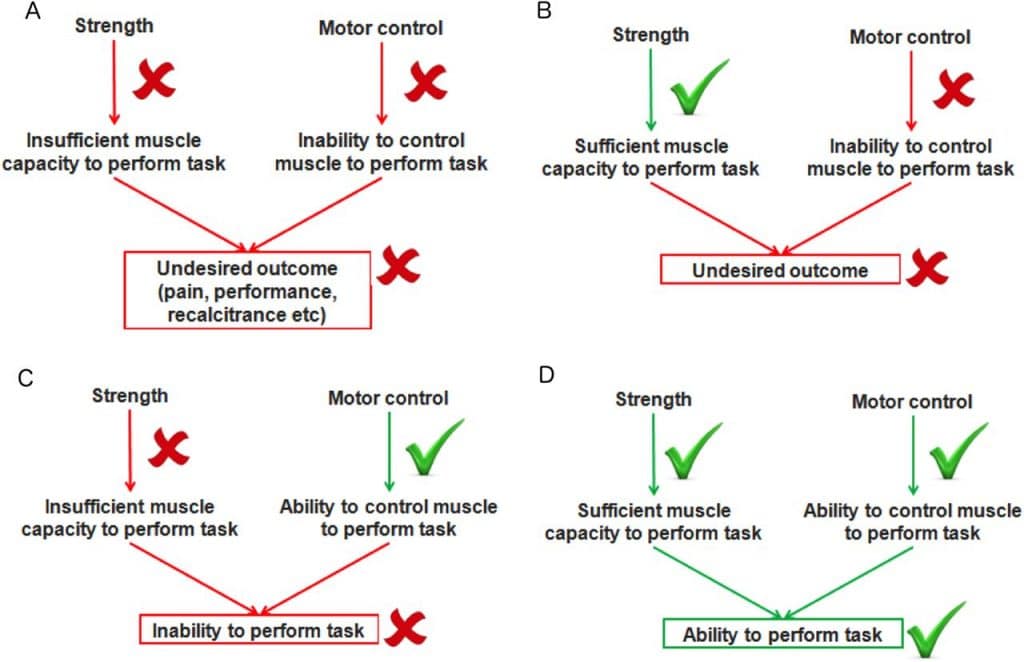
As we discussed, our brains can change according to various inputs. Those inputs can alter the way our brain is wired, and it can alter the signals that our brains send out. Tendon neuroplastic training has evolved in an attempt to cut off the inhibitory outputs, or temper the excitatory outputs the brain is sending to the lower motor neurons which control our muscle-tendon units. Research has shown that exercises performed to match a visual or auditory cue (metronome) have the ability to diminish excitatory signals or remove the inhibition at the level of the muscle-tendon unit. This is in contrast to self-paced exercises which do not appear to have the same effect on the brain’s signaling pathways. So, if you were told to go do 10 sets of a particular exercise, without cues, then the brain’s outputs would not change. However, if your reps were guided by audio or visual cues it appears that the brain’s activity was altered.
Do you have questions regarding an Orthopedic injury or longevity?
Do you want to talk to an expert who can listen to you for 45-60 minutes and explain the options in detail?
Dr. Howard Luks offers remote guidance sessions to review your X-ray or MRI images and explain your options.
Dr. Luks has also received hundreds of requests for educational sessions on the topics discussed in his book, Longevity Simplified.
As we mentioned before, the implications of this are significant. We know that people whose pain subsided after physical therapy or surgery still have a strength deficit. That may be due to persistent cortical inhibition by the brain. Theoretically, if we are able to improve the signaling by the brain, then perhaps a shorter course of rehab is needed to improve your pain, and more important, your risk of developing recurrent pain may decrease as well.
This is a fascinating and exciting evolution in the rehabilitation of our patients who suffer from tendinopathy. If you have been in physical therapy for tennis elbow, a jumpers knee, achilles tendinopathy or rotator cuff related pain and have not had any improvement after 6-8 weeks then I would suggest you discuss this concept with your Physical Therapist. We all get smarter when we share information!











Simon Bartold
Hello Dr. Luks, thank you for this article and explanation of an area I have been interested in for some time. i wondered if I might have permission to reproduce this on my own website with full acknowledgement of you and the website of origin.
thanks and best
Simon
HI.. Simon, Yes, sure, as long as you can use canonical code — otherwise google punishes both of us ;-)