
Millions of people suffer from degenerative joint disease (DJD), or osteoarthritis(OA) of the knee. Degenerative joint disease of the knee is the cause of significant pain and disability. Many people do not clearly understand what degenerative joint disease is. Perhaps your doctor said, “It’s just degenerative changes”. That’s all well and good, but your knee hurts, and you do not know what your next steps are. Many questions need to be addressed.
- What is Degenerative joint disease?
- How do I treat it?
- Why does it hurt so much? Should I continue to exercise (see video below)?
- Will exercise make my degenerative joint worse (see video below)?
- Are there non-surgical alternatives to treat knee DJD?
- Do I need surgery for my knee arthritis?
Let’s start first with the causes of degenerative joint disease and then proceed with the commonly accepted, reasonable treatment alternatives available for joint pain sufferers. Any decision you make should be based on your quality of life … and not your X-ray or MRI findings. We treat patients… not MRI or X-ray findings!
What is degenerative joint disease?
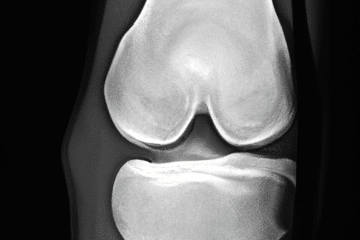
Degenerative joint disease, also known as osteoarthritis is due to the loss of cartilage within your joints. The articular cartilage is the cushioning that is on the ends of our bones. When we finish growing, that cartilage is fairly thick, it is firm and rubbery … and smoother than glass. For many reasons, we start to lose the cartilage, or we may suffer an injury which will cause us to lose our cartilage.
The causes of degenerative joint disease are numerous, some of the more common causes are:
- genetics — do you have a family member with arthritis?
- trauma — injuries can start a degenerative cascade to occur.
- nutritional — some think that vitamin D deficiency can cause arthritis
- mal-alignment — Are you bowlegged or knock-kneed?
- meniscus tears: loss of meniscus function (as a shock absorber) can lead to arthritis
Why does degenerative joint disease hurt?
If you lose enough cartilage or cushioning on the ends of your bones, then the bone underneath the cartilage will experience more stress. A degenerative joint disease is, by definition, a loss of cartilage. Our cartilage can wear thin over time, even without any specific injury to a joint. The most common causes of arthritis include genetics …. do your parents have it? Knee joint arthritis can also be caused by previous injuries, previous surgery, meniscus tears, ACL tears, and other more rare diseases.
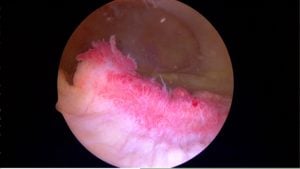
The pain due to DJD is caused by inflammation, or “synovitis.” Therefore, managing the pain of osteoarthritis is all about managing the inflammation or “synovitis”.
The synovium is the tissue which lines the entire inside of our joint. Usually, the synovium is thin and produces just enough fluid to allow our joints to move without pain or friction. In patients with degenerative joint disease or osteoarthritis, the synovium can become inflamed. That inflammation itself is the cause of significant pain. If the synovium is inflamed it may manufacture more fluid than normal and that’s why many of you have a warm, swollen knee — or as you may refer to as “water on the knee”. The most common cause of knee swelling is osteoarthritis. The latest non-surgical procedure available arthritis pain sufferers is a selective arterial embolization. It works by decreasing the inflammation within the knee by minimizing the blood supply to the synovium. The early results have been very promising. If interested read our post on arterial embolization for knee arthritis.
If your bones are not protected by cartilage they may experience more stress. That stress can lead to stress reactions or stress fractures which can cause severe pain. If you have had an MRI and they mention bone marrow edema — that means fluid or inflammation in the bone itself. Bone marrow edema is a common source of pain. If your X-rays do not show bone on bone arthritis, but you have bone marrow edema, then a procedure called a subchondroplasty might ease your pain significantly.
Can I exercise if I have osteoarthritis?
The video below shows the other list of treatments our patients utilize to treat their knee pain.
Degenerative joint disease treatments
Treatments and recommendations vary depending on how severe your pain is, your age, your activity level, and any other medical problems you may have.
Note: Any medication or supplements mentioned should be reviewed with your primary care doctor before starting them since they can interact with other medicines or they may not be indicated because of an underlying medical problem you have.
Do you have questions regarding an Orthopedic injury or longevity?
Do you want to talk to an expert who can listen to you for 45-60 minutes and explain the options in detail?
Dr. Howard Luks offers remote guidance sessions to review your X-ray or MRI images and explain your options.
Dr. Luks has also received hundreds of requests for educational sessions on the topics discussed in his book, Longevity Simplified.
- Lifestyle changes: Many people will experience relief from simply slowing down. Shorter walks, shorter runs, switching to a bicycle or swimming for exercise etc. Keep track of your activity. Try to increase your walking and aerobic capacity. Consider a Fitbit to monitor your activity. These trackers are great for helping you stay on course. Research has shown that exercise, specifically light weights or resistive training can minimize the pain of osteoarthritis or degenerative joint disease.
- Weight loss: I know, I know… BUT … for every one pound you lose, you will take 4-7 pounds of force off your knee!! Therefore even a relatively small weight reduction will result in significant pain relief. I have had many people cancel their knee replacement surgery after they lost 20-30 pounds.
- Braces or sleeves: Compression sleeves can provide meaningful relief of pain for many. We believe that compression sleeves improve knee pain because of a biofeedback mechanism. When you purchase one, if it is tight enough to stay on, it is tight enough… do not get a sleeve that is too tight. In this post I review the compression sleeves I see most commonly in the office.
Supplements and Vitamins
*Note: Many now believe that supplements have little role in managing knee pain. Despite that, the most popular supplements our patients are taking include:
- Vitamin D: Get tested. Know your level.
- Curcumin: Curcumin has many anti-inflammatory properties.
- Fish Oils: Fish oils contain chemicals which act in a similar way that aspirin or other NSAIDs do. Check with your doctor first since in can interact with other medications. Here is a rather scientific, but complete description of the benefits and side effects of fish oils and why they might work.
- glucosamine/chondroitin sulfate: Chondroitin Sulfate is the most commonly taken supplement. Some recent research shows that it may work to limit pain… but it will NOT regrow cartilage. A recent roundtable discussion among Orthopedic Surgeons show that they would take it too.
- Tart cherry juice There are many patients I have seen who enjoy the benefits of tart cherry juice.
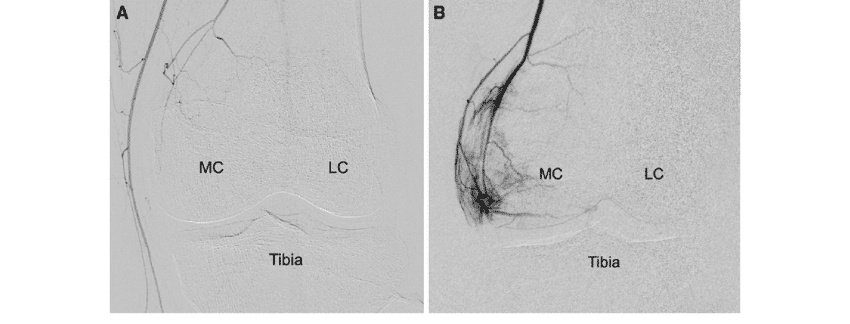
Selective Arterial Embolization
The pain of arthritis is often due to inflammation of the lining of the knee joint. That inflammation is often due to the fact that your body grew too many new tiny blood vessels to nourish the synovium around the swollen and arthritic areas of your knee. Recent research shows that selectively eliminating those extra blood vessels can lead to nearly complete relief of the pain from arthritis for 6 years or more.
- Injections: Nobody likes to receive an injection… and yes, they hurt — but they might give you significant relief. The options available to us include:
- Cortisone or steroids. These potent anti-inflammatories once injected will usually result in significant pain relief which can last for a few months. You must check with your physician first about potential interactions with other medications. If you are a diabetic, cortisone injections WILL make your blood glucose rise!
- Hyaluronic Acid : Examples include Synvisc, Orthovisc, Hyalgan, etc… Many people refer to these as gel injections. Some people mistakenly believe they are cartilage injections. They are not. Hyaluronic acid injections might improve your pain for upwards of 4-8 months. They are effective for most people… but not everyone.
- Platelet Rich Plasma or PRP: PRP is prepared by collecting a sample of your blood, placing that sample into a centrifuge and then taking off a certain layer and injecting it into your knee. Recent scientific literature shows that it may work to limit your pain significantly . PRP, or platelet-rich plasma injections, involve the injection of your own concentrated platelets, protein-releasing bodies, and other healing growth factors that can aid the body in resolving certain inflammatory conditions and can heal worn out tissues. It is an office based procedure where a small amount of blood is collected from you — the sample is prepared in a special apparatus placed into a centrifuge and then injected back into the site to be treated. In prior years PRP was investigated for the treatment of tendon-related disorders such as tennis elbow. PRP has received a lot more attention recently as an alternative to minimize or alleviate the pain associated with arthritis of the knee. In a recent study published in the The American Journal of Sports Medicine it was shown that PRP or Platelet Rich Plasma was effective for alleviating or improving the pain from arthritis of the knee. Further studies have shown that PRP injections may slow the progression of your osteoarthritis.
- Exercise: Resistance exercise and Minimal impact exercises such as rowing, swimming, and walking help alleviate the pain of arthritis and improve the strength of your legs… and your heart will be happier too. The research is also very clear in this area. Exercise will not make your arthritis worse. Perhaps exercising too much might cause more pain, but that does not mean that you are causing arthritis to become more severe. The research has also shown that people who remain active, and actively exercise are able to delay surgery for their degenerative knee pain for many years.
- Physical therapy: Either physical therapy, a pool program, or a gentle land-based exercise program can improve your pain and delay the need for more aggressive treatments. For those of you who are looking to start an exercise program than starting with a trained professional such as a physical therapist is a great place to start. Again, physical therapy is not going to cure your arthritis or degenerative joint disease, but for most of you it will improve your pain and thus improve your quality of life.
- Surgery:
- Arthroscopy: Tread lightly when someone recommends an arthroscopy or “scope” to “clean out” an arthritic joint. The results are usually poor, and the research is fairly clear that arthroscopy has a very limited role in the management of degenerative joint disease… at best. Most insurers and Medicare will not cover the surgery if the primary diagnosis is osteoarthritis.
- High Tibial Osteotomy: This is a procedure offered to young patients with arthritis limited to one side of the knee joint. It involves cutting the tibia and changing the alignment of the leg to take the pressure off the side of the knee that is arthritic. Visit this page for more information about a high tibial osteotomy.
- Knee replacement: Knee replacement is, unfortunately, the only definitive procedure we have to “treat” degenerative joint disease which has not responded to other treatments. Here is an interesting video to see. It is a video from a patient, where they offer their perspective on a knee replacement procedure. If the pain and disability is significantly interfering with your quality of life then a knee replacement might be a good option for you. Knee replacements can be partial, or “total”. A knee replacement is a big procedure, and you are a key member of the team. You need to be physically and emotionally prepared for your knee replacement, ready to assume the risks of surgery and be ready to work hard in rehabilitating your new knee. You need to find a surgeon who does a reasonable volume of joint replacement and doesn’t dabble in joint replacement surgery … volume matters and diminishes the risks of complications in knee and hip replacements. The NY Times published an opinion piece on the issue of the treatment of osteoarthritis and knee replacements that you may wish to review.












Alicia
I had surgery to repair a torn SCI and complete meniscus tear about six years ago. I’m overweight and have recently started to increase my activity level. I’m finding that I have significant discomfort after exercising and pain in the front inside of my knee when I bend at the waist. Does this sound like o set o f arthritis?
It is possible… it is also possible that your thigh / and hip muscles are weak.
Jeff
I am a 52 year old man who has had 2 scopes done on my right knee when I was in my 20’s. I have been having increased pain over the past few years. I had a cortisone shot that did more harm that good. I recently had an MRI and here are a portion of the results:
FINDINGS: “Moderate degeneration with chondrocalcinosis medial meniscus. Mild fibrillation fraying noted of the free edge. Chondrocalcinosis also noted of the lateral meniscus. There is studding of low signal intense calcium deposit within the cartilage of the lateral knee compartment. Articulating cartilage caliber of the lateral and medial knee compartments otherwise intact. Mild chronic sprain and thickening superior tibial collateral ligament. Similar-appearing low signal intense calcium studding noted of the medial patellar facet articulating cartilage. Mild marginal osteophytes patellofemoral joint. Minimal lateral patellar subluxation and tilting noted.”
I exercise 3 to 4 times a week and have lost over 40 pounds in the past 2 years. Labs show normal levels in all categories.
General Thoughts? I hope I won’t need a new knee, but if it gets rid of the pain, I may consider it.
CPPD can cause pain, especially if arthritis is present too. Not sure what your question was.
June Carr
hi im a 40 year old woman with this condition but my counsultant wont do anything all i was told was to lose some weight and some physio …. ive been suffering for over 6 years now i tried to lose weight but my chrons disease is making me put on weight is there anything i could try to ease the pain and stop the locking and cracking .
Did you try the physio? Perhaps a compression sleeve? Chondroitin Sulfate? You may even want to try the HA injections too. I can not make any formal recommendations without see you in the office first.
Good Luck
Jo Austin
Age 72….I twisted my left knee in nov 2015 doing an abrupt stop/twist to go back in the kitchen. Knee swelled and remained swollen. By Dec hurt to walk due to pain. Pain continues and it hurts each time I put my foot down. Pain is just below the knee cap on the inner not outer side of knee….(below the hinge part). Had it exrayed and saw dr. He chalks it up to arthritis. Xray shows some loss of cushion but not like bone is touching. Also reference to meniscus tear in the center. I wore a heavy knee brace for a few months….did some leg strengthening with rubber band where I pull with that leg. Absolutely no change in pain. It’s been so long now I fear that I’ve put myself out of knee alignment trying to compensate for the pain. When I lay down at night and lay the right knee on top of the left it’s painful to raise the left knee to a different position. Tried to do some walking outside my house…huge hill going down….pain….hill coming back up less immediate pain but it’s sensitive due to fact it’s in pain 24/7.
I work from home so knee hasn’t been over used and should have healed itself long ago. I bought a machine called Lightstim and tried using that to help healing. I’m lost trying to research all this. I don’t think arthritis just comes out of nowhere and I don’t have any sense of what I should do at this point. As it stands I’ve become disabled from this because I can’t walk but the smallest distance.
It’s painful all day every day over a year now? Your thoughts please
The pain of arthritis has to start sometime… This is a disease process that begins in our joints long before we will ever feel pain. It can take arthritis 10-15 years to progress to the point where it might hurt or ache. Some folks have horrible arthritic changes on X-rays and only mild pain. Some folks have mild arthritic changes on X-ray and terrible pain.
In someone with arthritic changes, it might take only a rather innocuous injury to cause pain… arthritic joints can be cranky – therefore they do not like even subtle injuries because of the cartilage damage. Time to talk to a few knee docs about your options going forward.
Jennifer
I am 52yrs and am in an awful amount of pain in my shoulder. I have been diagnoised by my surgeron I am bone on bone, No cartliage and need a full shoulder replacement. I am waiting to have this done, but all of a sudden the pain has increased so much so that it brings me to tears. I am taking Anti flames, & pain relief. I dont feel like going to my Dr as she cant do anymore for me. Any advise?? Many Thanks. Jenni.
Depending on how long it is until the surgery your surgeon can inject you or have a radiologist inject you using ultrasound or X-ray for guidance.
Please note… injections should not be done within 3 months of the surgery. They may increase the risk of infection.
Good luck
Lisa Weney
Hi: I just recently had Knee Arthloposty for which was supposed to be for a torn meniscus, turns out that the tear was so tiny that the doctor said it would have made it worse so he just cleaned it up and when I had my MRI in July he said it didn’t look like much arthritis in my knee but when he was doing the surgery he told me that I have entensive cartilage issues, he graded it 3 out of 4 I’m almost bone on bone and he said I would need it replaced. Is it normal still feel sore from the surgery and he also said I will have pain because of the cartilage problem. I’m considering the synvisc shots when I go back to the surgeon the end of January I’m hoping they help. Why does synvisc shots work for some and not others?
Thaat’s sadly the way it goes… many medications work for some and not others. Would have been nice to be able to avoid the arthroscopy.
Ken Plunkett
I have had CPK 3 to 4 times the maximum in blood test (600 – 850) for over a year. I also had X-rays and MRI’s that showed Degenerative Osteoarthritis in my knees, hips, lower spine and left shoulder over the past 5 years. Are the two related? One doctor told me DJD will probably progress to all my joints. Is there treatment to slow or stop this?
The OA can progress, yes. The CPK is not related to osteoarthritis. consult your primary care doctor to look into that further.
Dan Grasso
Seems you’re right. X-rays showed degenerative joint dz changes. It’s funny though, I had the same dx when I had a complaint of pain in the right foot a while back. X-rays showed the same thing. I changed the shoes I ran with to one with more cushioning and all the symptoms went away. I’ve taken a “painful” week and a half off running while doing other exercises. I’ve jogged a little at a slower pace and it seems to be okay. Thankfully, I don’t have any stress fx or something that would sideline me for a good while. I’ll continue to run, albeit slower, and see how that goes. I have a goal marathon in May that I WILL run. Thank you Dr Luks.
Dan Grasso
I’m a marathon runner and I began to feel a discomfort at the bottom of my left buttock, where the ischium attaches to the hamstring. I had all the symptoms of high hip tendonopathy. I told my doctor because I was afraid I might’ve had a stress fracture. I took the week off from running, but felt okay cycling and going on the elliptical.
I got the results of my x-ray. No stress fractures anywhere, just DJD. I was diagnosed with DJD in my R foot a while ago, and the discomfort went away when I started running with Hokas.
What do you recommend for hip DJD? Thank you.
Pain around the ischium might not be due to hip OA. Possible, but not definite. Sadly, there is no means of preventing OA from progressing. Your exam is just as important as your xray findings in terms of determining what the source of your pain is.
Terri Noland
Hi Dr.Luks,
I am a 49 yr old female who has had multiple ligament reconstructions (18 ttl surgeries 20+yrs ago). I am very active, and my job requires me to be on my feet all day. Hard to believe but my knee usually gives me very little trouble. About 30 days ago, I began feeling lots of popping and locking, and periods of intense pain. Saw a orthopedic physician in NYC, and after an MRI and Xrays, he recommended an arthroscope to clean out the joint and remove loose bodies and trim torn meniscus. I also, after all the above surgeries, still don’t have an ACL or PCL…who knew? Anyway…I did do a cortisone injection, but have not scheduled the surgery, as I am very reluctant to do any surgery after all of the failures. Do you think it would be a reasonable procedure to do, given the loose bodies and torn meniscus? Thanks.’
Terri
Glad we got to “talk” on Curely … look forward to seeing you.
Bano Murtaza
I am a female 60 years old living in Laguna Niguel , California. Due sever arthritis in both legs my movements are very restricted. Recent x-Rays of the knees showed there was no cartilage , only bone to bone contact. The doctor here have suggested knee surgery and have also recommended 4/6 weeks physiotherapy before the surgery. Since I am relatively new to the country I will appreciate if you could recommend a top doctor who has a lot of experience in the field in California. I hv consulted a doctor at Hoag hospital , Newport Beach.
I will be guided by your recommendation !
Thanks and best regards,
Hi Bano .. I do not know anyone in that region … sorry. Find someone who performs a fair number of knee replacements and has a low infection rate… don’t be afraid to ask them questions :-) !
Jacqueline Gillen
Thanks for the great info on your website. I’m a 72 y/o female tennis player….getting a PRP injection tomorrow for my knee…..first aspirating the Baker’s cyst…..initial injury was hyperextension playing tennis about 6 months ago. Your thoughts on resuming play after several weeks??
Dipak Joshi
Hello Sir
Very interesting article. I have completely torn my ACL and currently going thru physio. It has been six days and I am able to walk easily with mimimal swelling. I m using egg while and yellow with turmeric which has helped me so far in reducing swelling. One of my friend has recommended local stem cells and PRP injections which could avoid surgery. In your opinion can it cure this? and how safe is this. Also, what is the cost?
thanks
Regards
Dipak… It is certainly not curative… but it seems to have helped many with regards to pain. You need to discuss the specifics with the doctor who will perform the injections. Each preparation, and each PRP system is different. There is too little research out there to say it will definitely benefit you.
Good Luck
CHRISTINA
I am 59 yrs old. I have been suffering with knee problems for the last 15 yrs. I had arthroscopic surgery in both knees in 2002 and it greatly helped. A few yrs later I had Synvics injection which lasted several years and then again 4 months ago but really did not help. I have constant pain in my right knee and have been advised to have a total knee replacement. Recently I read about Prolozone Therapy. Would this be something that I should consider instead of a knee replacement?
No firm evidence to support it. You will be able to find people willing to inject a lot of different things into your knee. But you can not discount the placebo effect either. I can’t tell you what to do… but I wish you luck in your decision making.
Sam
I was just diagonised with degenerative deteriorating arthritis in my knee,my orthopedic surgeon thought that a meniscus surgery would work,so I had it done.when I came to the first thing I asked him was did it work,and he said no,unfortunately it did not.now my pain is worse then before the surgery.my doctor said I will have to have a total knee replacement but that I have to wait for 6 months,should I go get a second opinion?
The pain is very unbearable and I tend to want to fall if I don’t use my cane.please give me your opinion.thank you
Sorry Sam! That is one reason that many Orthopedists do not typically recommend an arthroscopy in the setting of advanced arthritis of the knee. There is a chance that your symptoms could worsen. Perhaps you could see a Rheumatologist for a series of injections while waiting for your knee replacement ???
Hobert Davis
I have degenerative joint disease in my knees,My Doctor has me on Oxycodone and it works real well but i am really scared of it I do not want to get to where I think I cannot live without it.
narcotics are not a great solution for arthritic pain management. It quickly can become a lifelong issue. Consider discussing alternatives with an Orthopedist.
Good Luck
Ron Kline
I have degenerative joint disease of the knees bilaterally would a knee replacement be a good choice to ease the pain in my knees? I have had one surgery on both my knees when i was young. I am 44 now? Please help really dont know what to do
Sorry Ron .. I can not say whether or not a knee replacement is appropriate for you or not without evaluating you.
Good Luck
Howard Luks
NameLeon
I have djd of the kne but also have sciatica both of which affect my left leg. My knee feels cold, not sure where the djd starts and the sciatica ends. It hurts to lay on my side either way, even if my legs are not touching. My sciatica is a lot better than it was when it first happened, but recently my upper thugh pain increased, will vitamin d and how much help? I am 58 and male.
Vitamin D alone will probably not help much. Tart cherry juice and a combination (tart cherry juice, tylenol and physical therapy) approach typically works best.