…and we should NOT think like mechanics.
Orthopedists and Twitter
Thanks to an orthopedic colleague, Dr. Katherine Burns, the Orthopedic community and any other interested parties on twitter were given a chance to observe for the first a well done live tweeting of an orthopedic meeting — focusing predominantly on the shoulder. Now, those of you have been around twitter for a long time, and certainly those of you who attended many healthcare meetings, and certainly healthcare marketing meetings clearly know that live tweeting of events is nothing new, however, from an orthopedic perspective — this was a big leap forward.
We are not mechanics… We treat patients, not MRI findings
The one upsetting issue is a theme that I see repeated over and over in the realm of orthopedic surgery, both in resident education, in what many people are told in offices around the world, as well as the focus of much of the literature that I read in the realm of shoulder surgery. That is the issue of *Mechanical Thinking*. Something is broken or torn so I must fix it!
A not insignificant focus withing the orthopedic literature — and certainly most of this meeting which was live tweeted focused on how to fix something, what techniques could be utilized to fix something, and what the overall results were from utilizing those techniques. The didactic sessions were followed by a laboratory session where the surgeon attendees were actually able to perform the surgery on cadavers in order to hone their skills. That’s all well and good. HOWEVER, this assumes that surgery was *necessary* or advisable in the first place. There was very little discussion centered about who needs surgery, when they need surgery, or why they need surgery.
A Patient Centric Approach
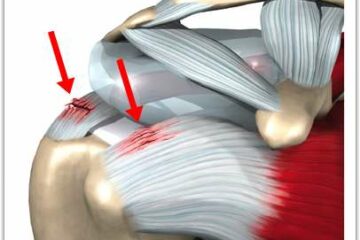
I received many questions through my website and certainly in my office in the form of second opinions where people put forth the issue that surgery was being recommended to repair a rotator cuff tear – – – yet they had relatively little if any discomfort. Many people offered that their pain was having little if any effect on their quality of life … and important Shared Decision Making principle. These were typically situations where they most likely had shoulder pain for a short period of time and were referred for an MRI (perhaps a little early), a rotator cuff tear was identified and purely mechanical thinking led to the recommendation for surgery. Since the recommendation, most of the patients who presented had already realized significant improvement in their pain and they were wondering whether surgery was indicated.
Orthopedic surgeons have been taught in the past that most tears *need* to be fixed. Again, mechanical thinking – – – if something is broken, we must fix it. We now know that this is probably not true. Why don’t I use the word probably? I use the word probably simply because we don’t have enough evidence to say with absolute certainty what tears need to be fixed and which tears do not need to be fixed. Very few surgeons would argue that acute or posttraumatic tears of the rotator cuff truly deserve to be fixed. However, many tears, or in fact most tears of the rotator cuff are attritional in nature — this is where the tissue simply wore out. The analogy that I frequently use is — your favorite pair of blue jeans you’ve been wearing for years. You look down one day or you feel a breeze around your knee and you look down and there is a hole in the front of your bluejeans. Did you rip it purposefully, did you lean on it or kneel on it or inflict some form of trauma to your pants :-) ? No, the tissue, or in this case the fabric simply wore out. So if that tissue is wearing out and we choose to repair it what’s the likelihood that the tissue has the ability to heal? If it is *successfully* repaired – – – because the tissue is degenerative, what’s to prevent it from simply tearing again? Once again, we simply do not have good answers to those questions.
Do I *need* surgery?
The same issue came up with labral tears. There was a lot of discussion about techniques to be utilized to fix labral tears, what techniques should be utilized in various age groups, etc. The number one number question in my mind, however, was not well addressed. That question of course is — “Do labral tears need to be fixed?” In many situations the answer is clearly yes. If your shoulder is unstable or dislocating then you need to have your labor repaired to minimize the risk of re-dislocation. If you are an overhead athlete and you sustain a labral tear, do you need to have that repaired? Occasionally the answer is yes. Unfortunately, some recent literature has shown that the vast majority of high-performance overhead athletes are not able to return to their prior level of function following a labral repair. Are surgeons informing these overhead athletes about these facts? There are many surgical success stories where we are clearly able to return a high-performance athletes back to their usual function. But it does not appear that labral surgery in this unique patient population is often successful … in weekend warriors and many high school or college players, a repair appears to be successful. But the margin for success is not high.
So, by and large this was a good week for the world of Orthopedics and Social Media. There are many more orthopedic surgeons on Twitter and other social media properties. This will ultimately prove to be a *good thing* for people searching for quality orthopedic information.
Eminence vs Evidence Based Medicine and Surgical Decision Making
On the flip side .. due to the persistence of Eminence Based Medicine in the community and the issue of purely mechanical thinking — I simply suggest that you temper your decision to proceed with a recommended surgery until you obtain a very clear understanding and an adequate discussion about the evidence that exists as to why the suggestion for shoulder surgery is being made — prior to you considering surgery. Have a clear understanding of what shared decision-making principles are. Perhaps even utilize the multitude of shared decision-making tools which are available to you on the Internet. If your surgeon is either not willing or capable of discussing the evidence or going through a shared decision making process with you — consider a second opinion— or moving on.












Hi, I had a surgeon look at me and my Mri. I sublexed a month ago in the turbulent river.. river sup surfing. I do this sport avidly and compete in a pro division. lots of water sports, water skiing, swimming.. diagnosis of MRI and surgeons ultrasound is: supraspinatus tendon is thinning w full thickness tear laterally , probable avulsion of anterior labrum. am doing PT. surgeon says it is probable I will dislocate in the future w my sports.. and that if I don’t get it fixed within a couple months the tissue can become irrepairable.. as tissue can turn to fat.. I heard this else where too.. I would like to try to repair myself.. and try my sup surf sport and water skiing when It is ” safe” ( originally prior to MRI I was given the 6 week mark on this) But now I am confused. I am going to send my MRI to another ortho and hope to be seen. In the mean time, trying to figure out the dos and do nots.. and the best course of action… if i loose a window where the shoulder can be fixed.. will i have to live w a shoulder that doesn’t work properly in the future? If I get it fixed, I have to go thru all that.. and will it work properly?
After a traumatic dislocation many/most people sustain a tear of the labrum on the front of the shoulder. For first time dislocators most sports docs would not recommend surgery. The issue is the potential for recurrence– meaning that the shoulder might dislocate again. The risk of having a second dislocation depends on someone’s age. The younger (under 25) the higher the risk Most sports docs would recommend surgery after your second dislocation. The labrum will be repairable for many years. It doesn’t become harder to repair, except if you start to have many many dislocations which starts to wear away the bone itself.
Hi Dr. Lukes,
I dislocated my shoulder in a fall a few weeks ago. My ortho ordered an MRI and it showed a SLAP lesion from 10 o’clock posterior through the superior and into the anterior labrum. My work requires me to lift my arm over my head to flip switches and push buttons. He recommended surgery to repair the lesion, but this would mean I’ll be off work for 6 months. This is my first dislocation and I’m 31 years old. Is trying physical therapy before surgery a good option for me? Also, I’m moderately active (running and lifting).
Most first time dislocators are not operated on…. Perhaps in an elite athlete, or in people who can not risk a second dislocation (tree climbers, roofers, rock climbers, etc) Most other people wait for second dislocation before considering surgery…. since the risk of a second dislocation becomes lower with age.
Dear Dr Luke’s,
I am so grateful to have found this page. On 12-8-17 I fell and dislocated my shoulder, the MRI stated that there is a -full thickness tears of distal supraspinous and infraspinatous tendons with approx 9mm of retraction. Tear measures 2.5 cm in AP dimension. Joint fluid extends through this defect into subacromial/subdeltoid space. A small joint effusion. I do not want surgery, is rehab a possibility for me? I’m 60 years young.
Thanks so much,
BC
Hi Bev…
The treatment of rotator cuff tears is often dependent on the 1. The cause of the tears and 2. The size of the tears.
Tears that occur after trauma– such as a dislocation are often treated surgically. They tend to heal well and result in a well functioning stable shoulder.
Tears that are chronic and or degenerative– meaning no trauma or injury are usually observed or treated with physical therapy.
Your tear is fairly large… two of the four muscles are involved. Your cause is acute trauma. Most all shoulder surgeons would agree that considering surgery might be your best option…. But only you and your doctor can make that decision. Please understand that I post for educational purposes and can not offer treatment advice as a physician in this forum.
Good Luck !
Dear Dr. Luks,
I appreciate you taking the time to help me understand my options, thank you. I don’t want to have the surgery that the doc recommended to me but I guess I’ll have to. I’ll be going for another opinion to another orthopedic Dr, because the initial Dr was just too eager to operate and wasn’t ordering a work up on my heart or any other precautions. I so appreciate your thoughts.
😉
Bev