
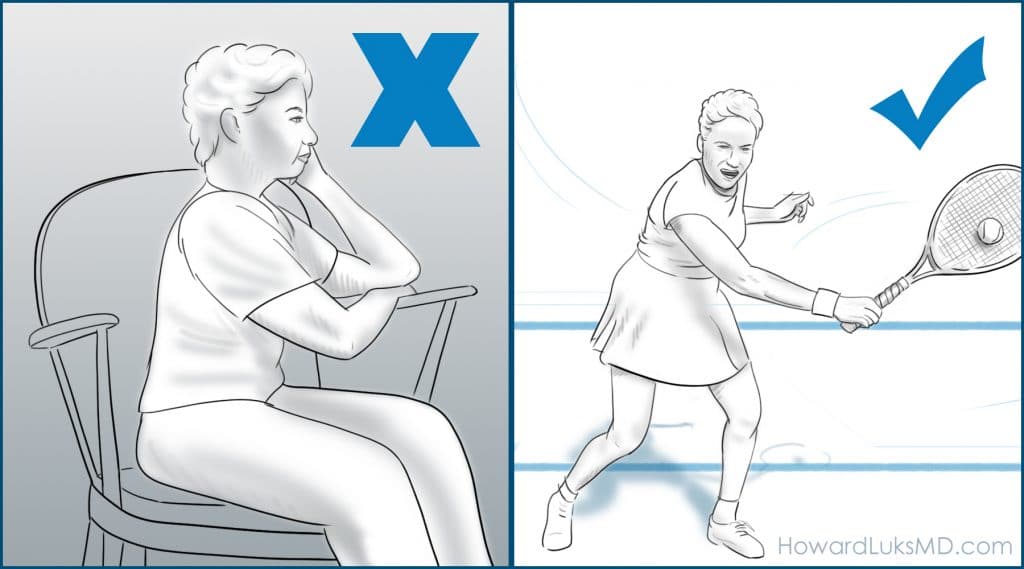
How many of you have been told to rest and stop running or exercising because you have knee arthritis? Far too many people (including healthcare professionals) believe that arthritis is caused by wear and tear. It’s only natural that you might assume that your knee arthritis pain will worsen, and arthritic progression will occur with exercise. I am here to tell you that you should not stop your exercise program because you are not saving your knee, quite the opposite, and you are increasing your risk of dying from all the most common causes of disability and death.
A recent study of runners and non-runners with osteoarthritis of the knee found that the runners did better, kept their natural knee longer before needing a knee replacement, and were generally happier than their non-running cohorts. Running at a self-selected pace does not worsen your osteoarthritis of the knee.
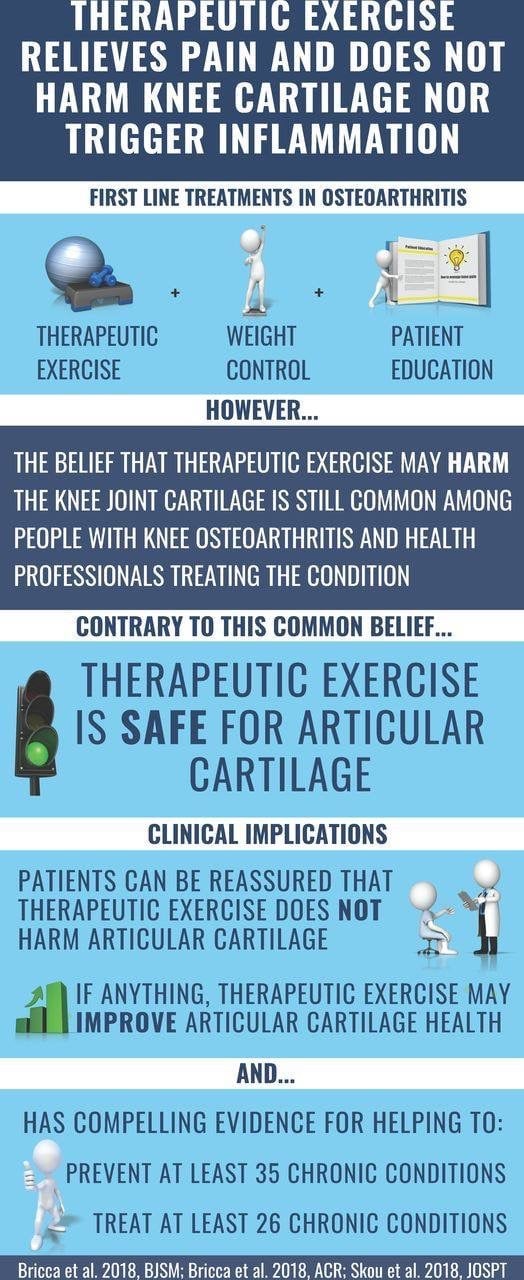
Osteoarthritis is very often not a mechanical wear and tear process. That grinding or sound that hear in your knee is not the rubbing away of your cartilage. You may want to bookmark this article on why arthritis occurs, and why exercise is probably the best medicine for it. Too many health care professionals counsel their patients to stop running, speed walking, elliptical, treadmill etc to save their joints. Most of the time you need to do just the opposite. The research over the years has been very clear. Therapeutic exercise does not worsen your arthritis and will very often improve knee pain due to arthritis.
Exercise has been proven to be the most effective treatment for early and moderate osteoarthritis of all of our joints. Exercise improves all-cause mortality and decreases your risks associated with muscle loss, frailty, sarcopenia and so on. We are going to walk through the current research and evidence-based recommendations for the management of arthritic knee pain.
Running may improve cartilage nutrition
What are the causes of osteoarthritis of the knee?
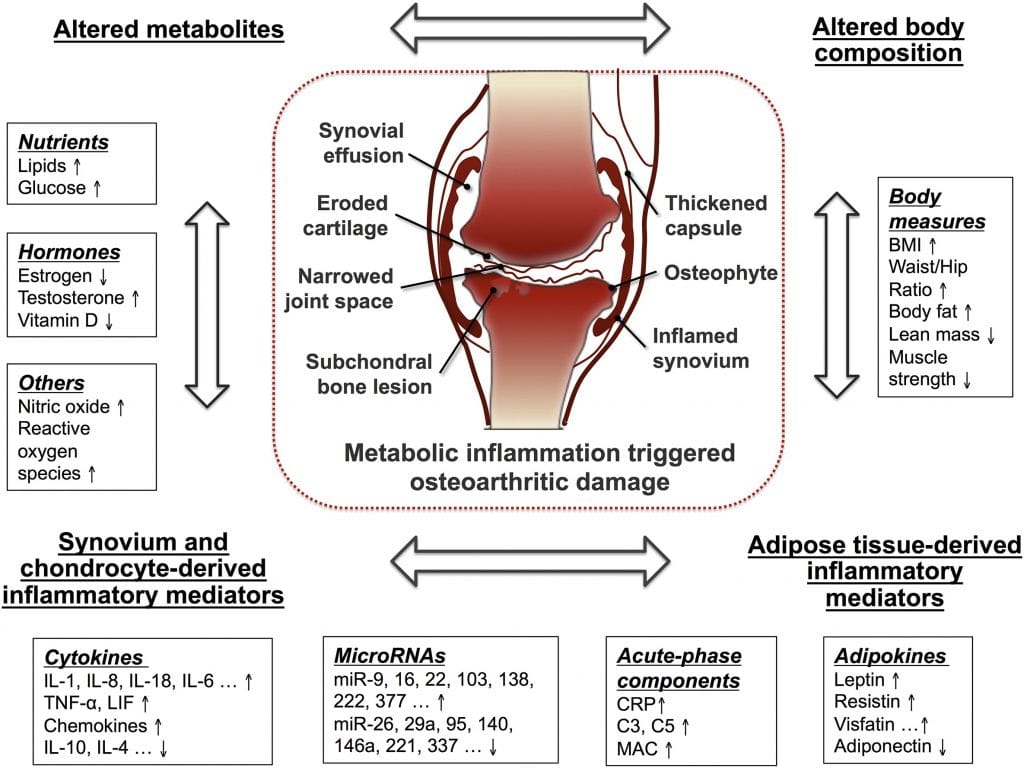
There are many potential causes of osteoarthritis of the knee. In people without prior injuries osteoarthritis is usually a biologically mediated inflammatory process…. what does that mean?!?
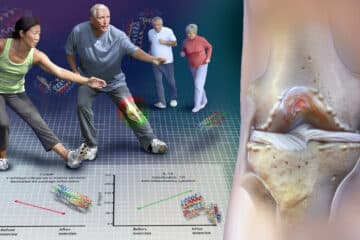
In our joints, we have 100s of proteins, cytokines, chemical, and other compounds which are made by the synovium, or the lining of the knee joint. When our joints are healthy, the chemicals in our joint support cartilage health and nutrition.
Then a switch flips… similar to the changes that lead to other disease states. That switch turns on the genes in our DNA that code for chemicals that are hostile to the health of our cartilage. So over time an increase in those hostile chemicals eventually causes the cartilage cells to die. That weakens the cartilage and its ability to withstand stress. That can lead to pain, inflammation, warmth, and swelling. One look at the picture below and you can see how complicated osteoarthritis can be.
Exercise has been proven to decrease the concentration of these hostile proteins and compounds in our knees. In this study, IL-10, a cartilage protective chemical in the knee was produced in response to exercise. In addition, the concentration of a compound called COMP decreased within the knee. COMP is a protein that is felt to be a biomarker of cartilage degeneration. This study shows that COMP levels in the blood increase during exercise but quickly return to baseline. Therefore the increase in COMP in the blood does not seem to reflect a negative effect on an arthritic knee. Other research studies show that the concentration of COMP within the knee decreases with exercise. Therefore, exercise might cause the COMP within the knee to be pushed into the bloodstream, or lymphatic system with exercise. Decreased COMP within in the knee, combined with an increase in the concentration of Interleukin-10 appears to show that exercise is not harmful to cartilage, and may in fact be beneficial. This research shows that running was associated with a decrease in the cytokines or the chemicals in the knee associated with cartilage wear and degradation.
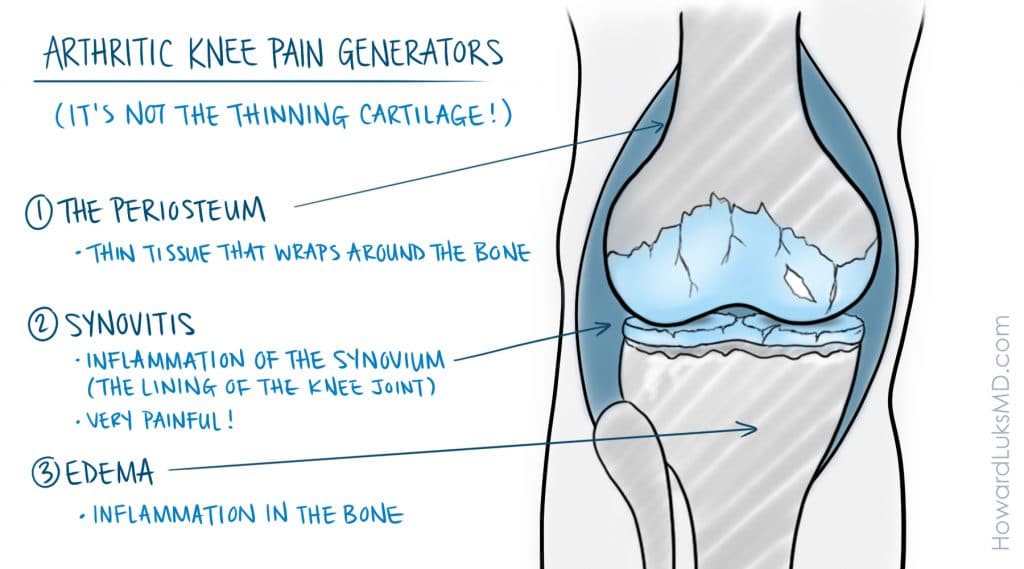
The pain in your knee is not often due to the loss of cartilage. Plenty of people lead very active lives with bone on bone arthritis changes.
What are the symptoms of knee arthritis?
The symptoms of arthritis of the knee can vary significantly. With mild arthritis, many people will have an ache associated with walking, stairs, or running. The location of the ache or pain can be on the inner side of your knee, the outer side, or even in the back of the knee.
Osteoarthritis in some people will produce swelling, or what is commonly referred to as “water on the knee.” Therefore some of you may have swelling of the knee while others will not. Depending on the location of arthritis within your knee it can feel like the knee wants to give way. A feeling of griding or “crepitus” is a common complaint. When the inflammation due to the arthritis increases, you may have pain in the knee at night. That’s why you may reach for a pillow to put between your knees when you sleep.
What are the causes of knee arthritis?
The cause of osteoarthritis of the knee is not entirely clear. Very different clinical pictures emerge when we see people in our offices and clinics. Some of you have mild arthritis that does not bother you much. Arthritis might progress or worsen slowly over decades, or it might progress more rapidly. In some, the pain you have might be minimal, and in others, the pain might be severe, regardless of how your X-rays look. That means that we have some patients with mild arthritis on an X-ray but they have severe pain and swelling. Others might have only a little pain despite X-rays that show severe arthritic changes.
The burden of osteoarthritis has been increasing across the globe. This is similar to the increase in chronic diseases such as dementia, high blood pressure, Type 2 Diabetes, and heart disease. All of the tissues in our body, including our cartilage are sensitive to our dietary intake. Metabolic issues are felt to have a causative role in the development of osteoarthritis and other chronic disease states. The earlier in our life that we realize this, the better off we will be. This post goes into more detail about the effect of our diet on our joint health and overall health. What might cause those genes in our DNA to become active? Good question… It may be coded in your DNA.
So if your parents have osteoarthritis your risk for getting it is higher. Like other chronic diseases you have heard me talk about, OA is similar in that it may be caused by poor metabolic health. It may also have been caused by an injury that occurred 20 years ago. One bleeding episode in the knee can initiate the process. Surgery can initiate an arthritic process too. Having a meniscus tear, and certainly having that tear removed compounds the problem. That adds a mechanical issue to the biological inflammatory issues- the perfect storm for OA and a good reason to avoid meniscus surgery if you can.
Certain experiments have proven that the concentration of those nasty chemicals in our knee will go down after running, or resistive exercise. Studies have also shown that the health of our cartilage is positively affected by running. Our cartilage seems to like the cyclical loading associated with certain activities. Most studies have shown that the chemical composition of cartilage is not adversely affected by exercise. While many studies show that knee pain from arthritis improves with exercise, the exact reason why is yet unclear.
Can I exercise with arthritis of the knee?
For more than 2 decades, the research has clearly shown that exercise is of benefit in people with osteoarthritis of the knee. Exercise improves pain, strength, and decreases muscle atrophy. Exercise can improve your quality of life and help delay the need for surgery. So… if someone tells you to rest because you have osteoarthritis… kindly say no. Osteoarthritis is not caused by walking too much or low impact activities. If your arthritis pain is due to severe osteoarthritis then you may need to consider other treatments above and beyond exercise.
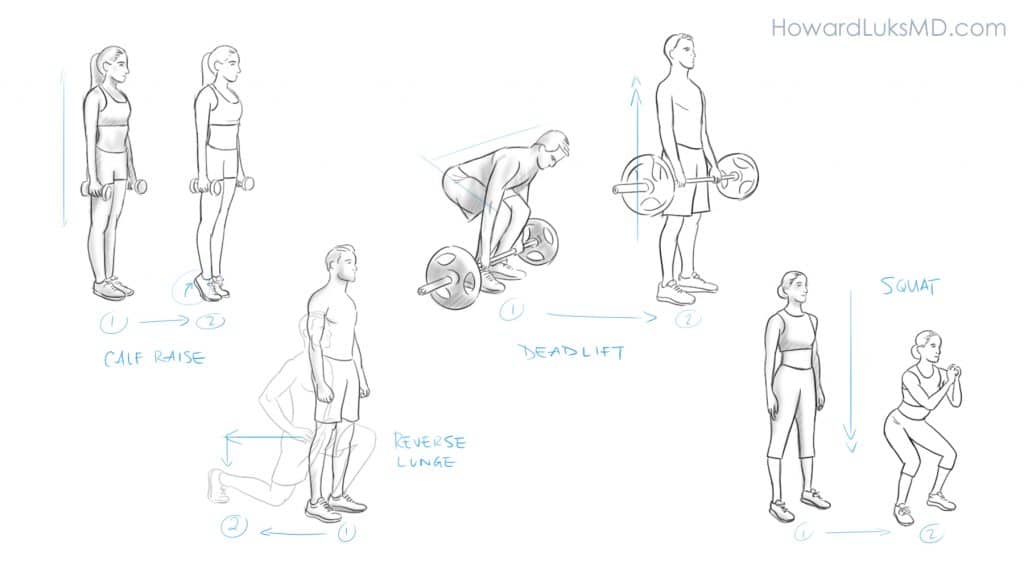
A proper exercise program to combat the age-related changes that we all experience will include aerobic exercise (walking, running, biking, swimming, etc), resistance exercise, and balance exercises. These different forms of exercise help minimize the risk of developing age-related muscle loss (sarcopenia), heart disease, dementia, type 2 diabetes, hypertension, and so on. This post on our site goes into more detail about the specific exercise programs we should be interested in to optimize our lives for longer healthspan.
Running and arthritis of the knee
Recreational running, even for those of us who have been running 20 miles a week for 40 years has NOT been associated with an increased risk of developing osteoarthritis. Study after study reveals there is no conclusive evidence that running causes osteoarthritis of the knee; in fact, running may actually slow the functional aspects of musculoskeletal aging.
Various initiatives have evaluated the risk of developing or worsening osteoarthritis of the knee in runners. For most people running is associated with improved arthritic symptoms (less pain and disability) and more important, running has not be shown to cause more advanced osteoarthritis. Even as far back as 1986 early studies on runners showed that their bone density increased (that’s good) and there were no signs of increasing osteoarthritis in male or female runners.
Does knee arthritis worsen with exercise?
No, osteoarthritis will not worsen with exercise. Osteoarthritis, by definition, will worsen over time. But that usually takes many, many years.
The cartilage cells in your joints actually like cyclical loading associated with running, walking, and strength training. The cells inside your knee will manufacture anti-inflammatory compounds and cytokines in response to exercise. That’s why most people with osteoarthritis of the knee feel better once they get moving. Most of the people I see in the office are afraid to exercise. They think that pain implies that they are causing harm. That is not the case with osteoarthritis of the knee.
Humans die of very predictable diseases. Heart attacks, strokes, dementia, the complications of type 2 diabetes, metabolic syndrome, etc. Exercise, even just walking 6000 steps per day will decrease your risk of dying from these common diseases. Please do not stop exercising because you are afraid of harming your knee. If your pain level is under a 4 (out of 10) then you should continue with your exercise.
Osteoarthritis of the knee is associated with an increased risk of all-cause mortality. That means that exercise and maintaining physical activity is critically important for your health and well-being. Formal programs are starting to emerge across the globe to help people improve their quality of life with arthritis that is not yet severe enough to require joint replacement surgery. GLA (D) is a program developed in Denmark that has demonstrated significant success in mitigating a lot of the disabling aspects of living with osteoarthritis of the knee. Exercise and walking are important to decrease the risk of dementia, to lower the risk of heart disease, to maintain or decrease our weight, to clear the cobwebs from our heads, to decrease blood pressure, and improve your overall health. Exercise is the best medicine for a joint that has started to degenerate or become arthritic. You are NOT wearing out your cartilage by walking or running.
Keep on truckin’
Some day your arthritis pain will worsen to the point that you may need to consider surgery. Until then, stay as active as you can be. Your head, heart, liver, lungs, and emotional well being will all benefit from that activity.












Dear Dr. Luks,
I have read several of your articles endorsing exercise as a strategy for living with knee OA. They have given me renewed hope. I’m a 60 year old woman, with some hypermobility issues and joint problems since early menopause.
I am currently having physio sessions for inflamed gluteal tendon, severe knee OA and thumb joint OA. I take Accoxel (COX-2) and also supplements and have taken Naproxen every single day for at least two years (since arthroscopy surgery that seems to have worsened the knee). Nothing has calmed the inflammation enough to allow me to exercise beyond walking short distances.
All you say resonates with my experience of surgeons and rheumatologists here in Spain where I live: gloomy prognosis, need for surgery though ‘too young’, recommendations to stop exercising from the physio. I want to believe that if I start again with stretching, strengthening and aerobic exercise and an even healthier diet, I can climb out of this inflammatory cycle of pain and limitation. I wish I could make an appointment with you, but failing that, I will take your words to heart. Thanks so much for the inspiring and authoritative information you have shared.
Thank you for your kind words. I hope that you progress well.
Good luck!
Dr. Luk,
Thank you for your common sense approach to orthopedics. As an aging singles tennis playing ER doctor with increasing knee pain on the nights I play tennis my Orthopedist friend directed me to you with my question to her- Will continuing to play high impact high level tennis with several hundred split steps every other day decrease my longevity on the court? I play with much younger players and enjoy singles but am up on my toes and doing split steps long after most my age have stopped doing both. Your article says low impact exercises do not contribute to arthritis- how about singles tennis with hundreds of split steps? I would prefer not to transition to flat footed doubles without split steps.
What an informative article. I have just had a PRP injection in my left knee here in France where I live. Very little info was given to me so this has been a Godsend. Thanks so much.
Kind regards, Lesley Twist.